What is sudden unexpected death in epilepsy, and what causes it?
When 20-year-old Disney Channel star Cameron Boyce died of “sudden unexpected death in epilepsy” (known as SUDEP) in 2019, his parents had not even heard of the condition.
“We didn’t know about SUDEP. We have family members who are doctors who never heard of SUDEP,” Cameron’s father Victor said in an interview.
We were clueless, completely clueless. The first time we heard [of] SUDEP is when the coroner told us that’s what took our son.
Most of us have heard of epilepsy, a brain condition that causes recurrent and spontaneous seizures. Lesser known to the public is that seizures can lead to an uncommon but fatal complication known as sudden unexpected death in epilepsy.
What is sudden unexpected death in epilepsy?
Sudden unexpected death in epilepsy is when someone with epilepsy dies without any warning and there is no other cause found. It often occurs immediately after a night-time convulsive seizure. Victims are often found in bed and lying face down.
While this can occur at any age, it particularly affects young people – the average age at death is only 26 years.
The risk of sudden unexpected death in epilepsy is highest in those who have convulsive or “tonic-clonic” seizures. With these types of seizures, the muscles stiffen, there is loss of consciousness, and the body starts jerking rhythmically.
This can cause a fast heart rate, as well as long pauses to breathing, which decrease oxygen levels. These seizures can place a lot of stress on the body.
Even one convulsive seizure in the past year can increase the risk of sudden unexpected death in epilepsy. In one Swedish study, having one convulsive seizure and not sharing a bedroom (meaning no-one is there to intervene if a seizure occurs in the night) made the condition 67 times more likely than those who do not have convulsive seizures and share a bedroom. As the number of convulsive seizures increase, the risk of sudden unexpected death also increases.
GettyImages/Frazer Harrison
Sudden unexpected death in epilepsy is the leading cause of death from epilepsy and accounts for over 80% of epilepsy deaths.
While the overall risk of SUDEP is low, with about 1 in 1,000 people with epilepsy affected each year, this risk increases to 1 in 150 in those with poorly controlled seizures. The risk increases with time, as epilepsy is often a lifelong condition, and the longer the exposure, the higher the risk.
But these figures are thought to be an underestimate. Because deaths commonly occur at night, they aren’t often witnessed, limiting what information there is about the time of death – for instance, whether there a seizure right before death. Often, victims are found deceased in bed and a history of epilepsy is overlooked as the cause of death.
People with epilepsy often have other serious medical problems such as heart disease, which can make identifying the cause of death difficult.
Autopsy findings are often inconclusive or attributed to heart issues, as even among forensic specialists there is limited awareness that epilepsy can cause sudden death.
Do we know what causes sudden unexpected death in epilepsy?
It’s still unclear why one person can have hundreds of convulsive seizures in their lifetime and won’t die of sudden unexpected death in epilepsy, and yet another can die after only a handful.
We think this is because there are many different causes.
Looking at sudden unexpected death in epilepsy cases that happened in hospital, researchers found that in all cases, a convulsive seizure caused a “flat-lining” of brain activity, which stopped the heart beat and breathing – all within minutes, causing rapid death. Survivors in this study all received prompt resuscitation within minutes.
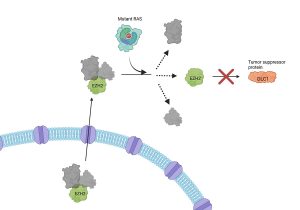
But in some people, seizures can trigger dangerous irregular heart rhythms – which may be another cause of the sudden death.
Some genetic conditions can impair how molecules responsible for electrical conduction in the heart and brain function. This can increase the risk of sudden unexpected death in epilepsy by making epilepsy and abnormal heart conditions more likely to occur together, heightening the risk of death.
Seizures can deprive the major organs of oxygen. Over time, repeated decreases in oxygen levels can cause damage to not only the heart, but also to the brain.
In people who died of sudden unexpected death in epilepsy, areas of the brain that control breathing and heart function had shrunk. Over time, this may increase the risk of sudden unexpected death in epilepsy by lowering the brain’s ability to control vital functions.
I or a loved one have epilepsy. What can we do?
Unfortunately, people with epilepsy and their families are often not counselled on sudden unexpected death in epilepsy and its risks. All newly diagnosed epilepsy patients should be informed about these risks at the time of diagnosis or shortly afterwards.
Individual risk varies. For most people with epilepsy, the overall risk will be low. Control of convulsive seizures is associated with the most significant risk reduction.
Most of the time this is achieved with the use of one or more epilepsy medications.
In people who don’t respond to epilepsy medications, brain surgery, implantable neurostimulators, or dietary therapies may offer some people hope in decreasing seizure frequency.
Read more:
What are ketogenic diets? Can they treat epilepsy and brain cancer?
It’s important to remember sudden unexpected death in epilepsy can happen to anyone with epilepsy – even those with well-controlled epilepsy.
Taking medications as prescribed and not missing doses, getting a good night’s sleep, avoiding alcohol and recreational drugs, and managing stress may reduce the risk of sudden unexpected death in epilepsy by making seizures less likely.
For some people who continue to have convulsive seizures, sharing a bedroom, or night-time monitoring devices may offer peace of mind and help with sudden unexpected death in epilepsy risk.
The causes of sudden unexpected death in epilepsy are many – understanding these will help develop targeted treatments. We need to develop tests that can identify people at high risk so we can optimise prevention strategies.
The development of night-time monitoring systems to identify dangerous seizures in the home and alert caregivers or emergency services is currently underway, and are sorely needed.