Fight Aging! Newsletter, December 11th 2023 – Fight Aging!
Fight Aging! publishes news and commentary relevant to the goal of ending all age-related disease, to be achieved by bringing the mechanisms of aging under the control of modern medicine. This weekly newsletter is sent to thousands of interested subscribers. To subscribe or unsubscribe from the newsletter,
please visit:
https://www.fightaging.org/newsletter/
Longevity Industry Consulting Services
Reason, the founder of Fight Aging! and Repair Biotechnologies, offers strategic consulting services to investors, entrepreneurs, and others interested in the longevity industry and its complexities. To find out more: https://www.fightaging.org/services/
A Longevity Industry Feature in Biopharma Dealmakers: Repair Biotechnologies, Deciduous Therapeutics, and More
https://www.fightaging.org/archives/2023/12/a-longevity-industry-feature-in-biopharma-dealmakers-repair-biotechnologies-deciduous-therapeutics-and-more/
Biopharma Dealmakers is a research news publication used by biotech and pharmaceutical startups to promote themselves and explain their work, published in association with editorial commentaries on the present state of the industry, as well as on specific areas of focus in research and development. It is published by Nature, and the way in which his typically works, under the hood, is that the editors decide on areas of focus for each issue and then reach out to selected companies related to that area of focus in order to invite them to pay a modest amount for inclusion. Technically this is a form of advertising wherein the Nature staff assists the selected companies in writing articles to discuss their research and development programs. The intended audience of that advertising is made up of life science investors and Big Pharma – publicity is ever useful!
However, this is also one of the few ways in which busy company leaders can be induced to explain their work in a format accessible to laypeople, and which is freely available to readers of any affiliation. So it can be an interesting read for industry observers. The last issue of 2023 includes a section on the longevity industry, and coverage of a few of the companies targeting age-related disease and mechanisms of aging that are currently interested in launching new initiatives or raising significant funding in the near future: Bioviva Science; Deciduous Therapeutics, a senolytics company; NIBEC; Rejuveron Life Sciences; and Repair Biotechnologies, the company that I co-founded. A few selected quotes follow, but I encourage you to take a look at the whole issue.
Biopharma Dealmakers, Volume 17 Issue 4, December 2023
Biopharma Dealmakers – a Nature Research publication – brings together life scientists, biotech and pharmaceutical professionals, and investors from across the globe. Biopharma Dealmakers offers readers themed editorial features that provide insights into dealmaking and industry trends. Regular editorial content includes biopharma deal round-ups, financing news and a collection of ‘business of science’ articles from the Nature Research catalogue. Biopharma Dealmakers also includes profiles of companies looking to partner or seek investment that showcases their pipeline products, technologies, therapeutic focus and partnering strategies. In this issue: Top 20 biopharma deals of 2023. Live forever: approaches to reverse aging. What are the drivers behind CNS deal flow? Oligonucleotide therapies broaden their reach. Make way for gene editing.
Editorial: The quest to turn back the clock
Delaying aging, restoring youth, regenerative medicine… whatever term is used, research aiming to target fundamental mechanisms of aging to increase life expectancy and quality has flourished in recent years. Ten years ago, researchers wrote a review that described hallmarks of aging, including genomic instability, stem cell exhaustion, deregulated nutrient sensing, mitochondrial dysfunction, and cellular senescence. Among efforts to target these hallmarks with potential therapies, those focused on cellular senescence have been at the forefront of industry activity, with more than 20 companies established in the past decade. In this piece, we highlight some of the progress and challenges for a selection of these companies.
Repair Biotechnologies: Developing therapies to degrade free cholesterol
Cholesterol is largely manufactured in the liver and transported throughout the body via a system of carrier molecules such as low-density lipoprotein (LDL) particles. Inside cells, cholesterol is esterified to provide protection from the toxicity of free cholesterol. Local excesses can overwhelm this protective mechanism and cells have no internal mechanism for degrading cholesterol. “When your system of transport breaks down, which happens in obesity and aging, localized excesses of cholesterol form. Our data show that the consequent toxicity is an important cause of downstream damage and disease.” No current therapeutics directly target free cholesterol. While lifestyle changes, statins, or PCSK9 inhibitors can dramatically reduce LDL cholesterol levels to lower risk of atherosclerosis and slow its progression, they do not significantly impact free-cholesterol excess or reverse the damage caused by free cholesterol. “Getting rid of excess free cholesterol was impossible until our approach to effectively target it.”
Established therapies focused on lowering LDL cholesterol cannot meaningfully remove established plaques, but Repair’s animal studies have shown a sizeable reversal of plaques following gene therapy mediated clearance of free cholesterol. The company is now finalizing its formulation and preclinical studies. Repair is also developing a therapy for NASH, which affects 3% to 6% of the US population, being more prevalent in patients with metabolic disease and obesity. It progresses from inflammation and fibrosis to cirrhosis in approximately 20% of cases and is associated with increased overall mortality. There is no US Food and Drug Administration (FDA)-approved therapy for NASH, and, like atherosclerosis, its progressive pathology is largely irreversible. Repair’s gene therapy reduced liver-tissue free cholesterol in mouse models significantly after only a few days, rapidly reducing key serum markers of liver damage. Moreover, hallmarks of NASH pathology including liver inflammation, insulin resistance and, most importantly, liver fibrosis were all significantly reduced following an 8-week therapy.
Deciduous Therapeutics: Restoring immune surveillance to tackle age-related diseases
Researchers discovered that a subtype of cells that sit between the innate and adaptive immune system were dramatically dysfunctional where senescent cells were accumulating. They m showed in two different mouse models of disease that the number and function of these invariant natural killer T (iNKT) cells was significantly reduced in tissues with high levels of senescent cells. Initial work showed that a tool compound, alpha-galactosylceramide (αGalCer) could be used to activate iNKT cells and reduce senescent cells in adipose tissue, leading to durable improvements in blood glucose levels, insulin resistance and HbA1c levels in diet-induced obese mice.
Subsequently, to demonstrate the widespread utility of immune-based senolysis, the company applied the approach to a severe model of pulmonary fibrosis. In this study, a single treatment at the peak of disease resulted in the ablation of senescent cells in the lung and attenuation of key fibrotic and inflammatory markers, which ultimately resolved fibrosis. Deciduous Therapeutics has used computational assisted design to synthesise a suite of proprietary therapies that could be used in the clinic to re-activate tissue-resident iNKT cells. To date, the company’s lead program has shown single-dose efficacy in resolving both metabolic and fibrotic diseases along with a favorable safety profile at doses significantly higher than the efficacious dose.
Klotho as a Biomarker of the Influence of Lifestyle Choice on Health
https://www.fightaging.org/archives/2023/12/klotho-as-a-biomarker-of-the-influence-of-lifestyle-choice-on-health/
Klotho is a longevity-associated protein that operates both within the cell and also as a circulating signal protein. It is longevity-associated in the sense that upregulation increases life span and downregulation reduces life span in mice, but also in the sense that measured klotho levels correlate with health and life expectancy in human epidemiological studies. Klotho may largely operate by maintaining kidney function into late life, but researchers have found that it may also help brain cells resist the harmful effects of an aged environment.
In today’s open access paper, the authors make the interesting point that while epigenetic clocks are receiving attention as a potential way to assess the effects of lifestyle interventions on health and aging, there is in fact a great deal more existing evidence for the use of klotho as a biomarker in this context. Klotho may be a good enough reflection of the state of fitness, diet, and metabolic health to be used as a way to test compliance with lifestyle change in studies, or to assess the degree to which a given lifestyle change is in fact improving long-term health in any given individual.
The Longevity Protein Klotho: A Promising Tool to Monitor Lifestyle Improvements
With the global population aging, the number of people with multiple chronic health conditions has been rising because medicine still focuses on treatment rather than prevention. It is estimated that one in three people in the world lives with two or more chronic diseases. One way to prevent and even reverse chronic diseases is through lifestyle changes through health promotion and education. This also helps delay the onset of geriatric syndrome (frailty, cognitive decline, and reduced performance in the activities of daily living scale). This is why a new discipline of medicine has emerged to specifically address this issue: lifestyle medicine.
The American College of Lifestyle Medicine (ACLM) promotes a science-based approach that integrates lifestyle factors to prevent and treat chronic conditions. There are six pillars of lifestyle medicine: nutrition, physical activity, stress management, restorative sleep, social connection, and avoidance of risky substances. The goal of this discipline is not only to prolong the lifespan but to increase the healthspan by reducing the morbidity span. A study estimated that adherence to four or five low-risk lifestyle factors (diet, physical activity, alcohol intake, etc.) at age 50 could extend life expectancy free of major chronic diseases (cancer, cardiovascular disease, or diabetes) by 7.6 years in men and 10.6 years in women when compared to people with no low-risk lifestyle factors
Healthspan is defined as longevity without diseases and is often associated with a higher quality of life. Healthy longevity is a World Health Organization (WHO) priority. Chronological age, the number of years a person has been alive, is a great predictor of disease prevalence and mortality risk but is unchangeable. On the other hand, biological age is variable and measures the accumulation of physiological damage in individuals, meaning that two individuals of the same chronological age can have different biological ages. Thus, a biological marker providing a quantifiable overall insight into the patient’s current health status would be of great use.
A few longevity markers do currently exist, such as PhenoAge (algorithms to improve chronological age by adding 9 biomarkers found in routine blood tests) or GrimAge, which is an epigenetic clock that can evaluate the biological age of an individual using DNA methylation-based markers. These tests are reliable for determining biological age, but there is little literature linking them to healthspan potential and even less to each of the pillars of lifestyle medicine. A new biomarker, the longevity protein klotho, might become a game-changing tool for measuring metabolic health and predicting the potential for healthy longevity. This review introduces the klotho protein as a potential novel, cost-effective biomarker and integrative tool to quantify and monitor the health status of individuals adopting lifestyle behavioral changes and summarizes current knowledge on the extent of klotho regulation across the six pillars of lifestyle medicine.
Based on this narrative analysis, klotho is a very promising marker candidate for lifestyle medicine due to its potential involvement in the six pillars of lifestyle medicine. Although we have identified knowledge gaps that warrant further study (randomized trials) to better understand the use of klotho in monitoring the effect of a lifestyle change intervention, it has enormous potential to enable objective, quantitative, and rapid monitoring of the overall health and the healthspan of patients. Klotho could be used as a marker in clinical studies where it is difficult to control the entire patient environment. Klotho is easy to quantify and, in the case of age-related diseases, would be an excellent marker to follow, as some diseases show no perceptible symptoms for a long period of time.
VCAM1 and APOE Involved in Microglial Clearance of Amyloid-β
https://www.fightaging.org/archives/2023/12/vcam1-and-apoe-involved-in-microglial-clearance-of-amyloid-%ce%b2/
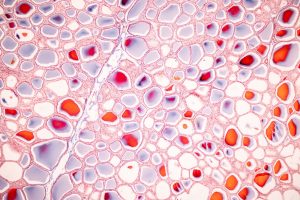
One of the characteristics of neurodegenerative conditions such as Alzheimer’s disease is the inflammatory activation and dysfunction of microglia. These are cells of the innate immune system distinct to the brain, analogous to macrophages elsewhere in the body. They undertake a similar portfolio of tasks, including chasing down pathogens, destroying errant cells, cleaning up waste and debris such as toxic aggregated proteins found outside cells, and aiding in tissue maintenance and repair. When microglia are in an inflammatory state, they are less inclined to aid in tissue maintenance and clearance of harmful metabolic waste. Further, changes in the signaling environment and other aspects of aging can interfere in the capacity of these cells to clear debris and waste even when they inclined to do so.
In today’s research materials, researchers describe some of the mechanisms that regulate clearance of misfolded, aggregated amyloid-β. Aggregation of amyloid-β is a feature of the early stages of Alzheimer’s disease, and is thought to cause the onset of later inflammation and tau aggregation. Alzheimer’s may thus be a consequence of an age-related failure of the balance between formation and clearance of amyloid-β aggregates. Increased production of amyloid-β may play a role, in its capacity as an antimicrobial peptide in response to infections, and so may reduced drainage of cerebrospinal fluid from the brain, but much of the focus is on reduced clearance by microglia. It is thought that ways to restore the clearance activities of microglia may slow or reverse Alzheimer’s disease in its early stages.
Scientists Unveil Promising Target for Alzheimer’s Disease Treatment
Alzheimer’s disease (AD) is a devastating neurodegenerative disorder that affects over 50 million people worldwide. A key pathological hallmark of the disease is the accumulation of amyloid-beta (Aβ) plaques in the brain, which leads to progressive decline in cognitive function. Microglia, resident immune cells of the brain, are thought to play a vital role in the clearance of Aβ plaques, a function that is impaired in AD.
The research team sought to investigate how microglia control Aβ clearance and how they become dysfunctional in AD. Through their elegant study, the team discovered that VCAM1, a cell surface protein on microglia, mediates microglial migration towards Aβ and promotes microglial clearance of Aβ. The team also discovered that another protein found in Aβ plaques, APOE, acts in conjunction with VCAM1 to mobilize microglia to Aβ plaques. The team further found that stimulating the “VCAM1-APOE” pathway reduced AD pathology in a mouse model of AD. These findings suggest that proper VCAM1 functioning is critical for microglial migration and clearance of Aβ.
The team also examined VCAM1-expressing microglia in the brain tissue of AD patients. Interestingly, AD patients exhibited elevated levels of soluble VCAM1 in the cerebrospinal fluid, which suggested dysregulated VCAM1-APOE signaling. This observation correlates with reduced clearance of Aβ by microglia. Collectively, the findings of the study implicate VCAM1-APOE signaling in the pathogenesis of AD and identify VCAM1 as a promising target for AD therapy.
The VCAM1-ApoE pathway directs microglial chemotaxis and alleviates Alzheimer’s disease pathology
In Alzheimer’s disease (AD), sensome receptor dysfunction impairs microglial damage-associated molecular pattern (DAMP) clearance and exacerbates disease pathology. Although extrinsic signals, including interleukin-33 (IL-33), can restore microglial DAMP clearance, it remains largely unclear how the sensome receptor is regulated and interacts with DAMP during phagocytic clearance. Here, we show that IL-33 induces VCAM1 in microglia, which promotes microglial chemotaxis toward amyloid-beta (Aβ) plaque-associated ApoE, and leads to Aβ clearance. We show that IL-33 stimulates a chemotactic state in microglia, characterized by Aβ-directed migration.
Functional screening identified that VCAM1 directs microglial Aβ chemotaxis by sensing Aβ plaque-associated ApoE. Moreover, we found that disrupting VCAM1-ApoE interaction abolishes microglial Aβ chemotaxis, resulting in decreased microglial clearance of Aβ. In patients with AD, higher cerebrospinal fluid levels of soluble VCAM1 were correlated with impaired microglial Aβ chemotaxis. Together, our findings demonstrate that promoting VCAM1-ApoE-dependent microglial functions ameliorates AD pathology.
Targeting Oxidative Stress to Provoke Greater Tissue Maintenance and Regeneration in the Aging Heart
https://www.fightaging.org/archives/2023/12/targeting-oxidative-stress-to-provoke-greater-tissue-maintenance-and-regeneration-in-the-aging-heart/
The heart is one of the least regenerative organs, and what limited ability it has to recover from injury is further diminished by age. This is of particular concern in the context of recovery from a heart attack, which leaves regions of scar tissue rather than functional tissue, weakening the heart. The best approach to this problem is to prevent heart attacks from occurring in the first place, which would have to be achieved by in some way halting and reversing the underlying processes of atherosclerosis and the growth of fatty lesions in the vasculature. There is enthusiasm for this goal in academia and industry, at least in principle, but very little concrete progress in departing from the futile focus on lowering LDL-cholesterol in the bloodstream, which can only modestly slow the progression of atherosclerosis, not reverse it.
Thus, a sizable fraction of the regenerative medicine community is interested in finding ways to provoke greater regeneration in heart tissue, largely with the primary goal of helping heart attack survivors to regain at least some lost function. Today’s open access paper is a discussion of the role of oxidative stress and cellular senescence in the age-related loss of regenerative capacity in heart tissue, with particular attention given to the function of progenitor cells in the heart responsible for regeneration. Researchers are looking for ways to reprogram the behavior of these cells, to reduce the impact of senescence, and it may be that oxidative signaling is a place to start.
Targeting the redox system for cardiovascular regeneration in aging
Lifespan has nearly doubled over the recent seven decades, but the final years of life come often with aging-associated diseases, most prominently cardiovascular disease (CVD) featured by progressive deterioration of cardiovascular structure and function. Aging imposes extensive changes on cardiovascular tissues that lead them toward a pathological state including hypertrophy, left ventricular dysfunction, arterial stiffness, and vascular dysfunction. Extrinsic factors, such as environment and lifestyle, and intrinsic processes, such as oxidative stress and inflammation, exacerbate DNA damage response, metabolic remodeling, and epigenetic drift, and thereby promote cellular aging in the cardiovascular system. These irreversible changes progressively impair the ability of cells to proliferate, which is critical to replace damaged cells that naturally accumulate in aged cardiac and vascular tissues.
During the recent decade, it is increasingly understood that the accumulation of the non-proliferating cells, so-called “senescent cells,” declines mammalian tissues and organ function. According to the emerging “adult stem cell senescence theory of aging,” stem cells and/or progenitor cells harboring in the heart and blood vessels or circulating progenitor cells, which replenish either preexisting senescent stem cells or specialized cardiomyocytes (CMs) and endothelial cells (ECs), become exhausted and lose their stemness during aging. The aging/senescence milieu suppresses endogenous regenerative and reparative mechanisms in the adult stem cells and progenitor cells, and also limits the success of cell-based regenerative therapies that aimed at repairing injured and dysfunctional tissues and restoring a youthful phenotype in the cardiovascular system. In a middle-size human study involving 119 humans with cardiovascular disease (32-86 years), more than 50% of tissue-specific cardiac progenitor cells (CPCs) exhibited the senescence phenotype.
Reactive oxygen species (ROS) have been viewed as pathological molecules that undermine normal cellular pathways by increasing oxidative stress. The cardiovascular system is principally vulnerable to reactive oxygen species (ROS) induced oxidative damage due to its high metabolic demand and low antioxidant defense capacity in aging. Single-cell RNA-Seq analysis of mouse aged cardiovascular ECs reveals transcriptomic reprogramming, including upregulation of ROS metabolic process in these cells. Not only in aged arterial ECs, single-nucleus RNA-Seq verify that oxidative responses are enriched in aged CMs in both primate and human hearts. These studies and beyond have demonstrated that these aged cardiac and arterial tissues exhibit a higher level of senescence-associated β-galactosidase staining and expression of pro-senescence genes including IL1β, IL17, and Type-I interferon (IFN-α). The relentless ROS production can also cause oxidative stress in cellular components, leading to cardiovascular stem/progenitor cell senescence and impaired proliferation and differentiation.
A mounting body of evidence underscores the significance of targeting redox machinery to restore stem cell self-renewal and enhance their differentiation potential into youthful cardiovascular lineages. Hence, the redox machinery holds promise as a target for optimizing cardiovascular regenerative therapies. In this context, we delve into the current understanding of redox homeostasis in regulating stem cell function and reprogramming processes that impact the regenerative potential of the cardiovascular system. Furthermore, we offer insights into the recent translational and clinical implications of redox-targeting compounds aimed at enhancing current regenerative therapies for aging cardiovascular tissues.
Progressing Towards Regulatory Approval of Veterinary Therapies Targeting Aging
https://www.fightaging.org/archives/2023/12/progressing-towards-regulatory-approval-of-veterinary-therapies-targeting-aging/
Veterinary medicine is typically less impeded by FDA regulatory costs than human medicine. A cynic would note that the publicity-related incentives operating on FDA staff and leadership are quite different in these two cases, with a great deal more attention given by the media to matters regarding human medicine. With the relative costs being what they are, a number of entrepreneurs in the longevity industry chose to work towards veterinary therapies targeting mechanisms of aging. One of those companies, Loyal, here reports on progress towards the FDA essentially agreeing to a regulatory framework for therapies targeting aging rather than specific diseases. On the human side of the house, you might recall that the primary analogous effort is the TAME trial and the lobbying surrounding it, a very expensive and slow-moving process that has yet to come to fruition.
Loyal’s approach involves adjusting a mechanism of metabolism that operates differently in large dogs versus small dogs, and which may provide a meaningful contribution to the well-known lifespan differences between breeds of different sizes. This treatment is thus intended for large dogs only. The FDA may or may not be considering the details of the specific approach used to be an important factor in allowing treatment of aging in dogs. The regulators may or may not reject a similar path to approval for other approaches, such as implementations of SENS-style repair of molecular damage. It remains to be seen as to whether a following company will be able to point to Loyal’s regulatory progress and expect the FDA to approve a different treatment intended to slow or reverse aging in dogs, or other animals, without picking a specific disease to focus on. Still, that is the goal!
FDA Center for Veterinary Medicine agrees Loyal’s data supports reasonable expectation of effectiveness for large dog lifespan extension
Loyal was only a few months old and about five people when we decided to begin by targeting the abnormally short lifespan of large breed dogs with a drug program we code-named LOY-001. LOY-001 extends lifespan in part by reducing IGF-1 to levels seen in smaller-breed dogs. The IGF-1 axis is one of the most well-studied longevity pathways. In model organisms from C. elegans to mice, reducing IGF-1 extends healthy lifespan, and increasing IGF-1 shortens healthy lifespan. In humans, certain centenarians have been shown to have genetically lower levels of IGF-1.
Today, I’m so proud to announce that Loyal has earned what we believe to be the FDA’s first-ever formal acceptance that a drug can be developed and approved to extend lifespan. In regulatory parlance, we have completed the technical effectiveness portion of our conditional approval application for LOY-001’s use in large dog lifespan extension. As there was no established regulatory path for a lifespan extension drug, we had to design from scratch a scientifically strong and logistically feasible way to demonstrate efficacy of an aging drug. This process took more than four years, resulting in the 2,300+ page technical section now approved by the FDA. It included interventional studies of LOY-001 in an FDA-accepted model of canine aging and an observational (no-drug) study of 451 dogs.
Our interventional studies with LOY-001 showed that the drug improved clinically-relevant aging parameters. We assessed these in laboratory studies using a dog model that represents accelerated aging. We then correlated those results with quality of life scores in the observational study, as independently measured by dog owners, and health outcomes as measured by veterinarians. This was key to show that the biological benefits of the drug are linked to clinically relevant outcomes. From our data, the FDA believes LOY-001 is likely to be effective for large dog lifespan extension in the real world. Once we satisfactorily complete safety and manufacturing sections and other requirements, vets will be able to prescribe LOY-001 to extend the lifespan of large dogs while we complete the confirmatory pivotal lifespan extension study in parallel.
The Pace of Epigenetic Drift is Slower in Long-Lived Species
https://www.fightaging.org/archives/2023/12/the-pace-of-epigenetic-drift-is-slower-in-long-lived-species/
Epigenetic drift is a measure of age-related change in epigenetic marks that alter the structure of packaged DNA in the cell nucleus, and thus control gene expression by making regions accessible or inaccessible to the translation machinery that produces RNA from gene sequences. Regardless of whether epigenetic drift is a form of damage contributing to aging, or a reflection of stochastic molecular damage within cells and consequent disarray in signaling and environment, one would in either case expect it to scale with species life span. Longer-lived species must show a slower pace of change in measures of aging, it would be surprising to find a measure for which this was not the case.
Epigenetic drift or “disorder” increases across the mouse lifespan and is suggested to underlie epigenetic clock signals. While the role of epigenetic drift in determining maximum lifespan across species has been debated, robust tests of this hypothesis are lacking. Here, we test if epigenetic disorder at various levels of genomic resolution explains maximum lifespan across four mammal species. We show that epigenetic disorder increases with age in all species and at all levels of genomic resolution tested. The rate of disorder accumulation occurs faster in shorter lived species and corresponds to species adjusted maximum lifespan.
While the density of cytosine-phosphate-guanine dinucleotides (“CpGs”) is negatively associated with the rate of age-associated disorder accumulation, it does not fully explain differences across species. Our findings support the hypothesis that the rate of epigenetic drift explains maximum lifespan and provide partial support for the hypothesis that CpG density buffers against epigenetic drift.
In Alzheimer’s Patients, Neuropsychiatric Symptoms Correlate with Neuroinflammation
https://www.fightaging.org/archives/2023/12/in-alzheimers-patients-neuropsychiatric-symptoms-correlate-with-neuroinflammation/
Chronic, unresolved inflammation is a feature of aging. It emerges from mitochondrial dysfunction and mislocalization of mitochondrial DNA, from visceral fat tissue, from senescent cells, and from a range of other maladaptive processes. Sustained inflammatory signaling is disruptive of cell and tissue function. In recent years, researchers have come to put a greater emphasis on the role of chronic inflammation in the onset and progression of Alzheimer’s disease. While it remains the case that protein aggregation (of altered amyloid-β and tau) is the primary point of focus in Alzheimer’s research and the development of treatments, inflammation does appear to have a central role in the pathology of the condition.
Earlier this year, scientists discovered that excessive brain inflammation is critical for disease initiation and can predict whether cognitively unimpaired elderly are at a higher risk of developing Alzheimer’s symptoms. This earlier research hinted at the importance of neuroinflammation in the pathological cascade involving other key players in Alzheimer’s pathology including amyloid beta and tau. Now new findings provide the first strong evidence that brain inflammation is also a direct cause of neuropsychiatric symptoms that often accompany Alzheimer’s-associated dementias.
In the new study, the researchers worked with 109 elderly individuals, the majority of whom had no cognitive impairments. Most of those individuals were, however, positive for amyloid and tau. By measuring levels of neuroinflammation, amyloid beta, and tau via brain imaging and comparing the results with clinical assessments of neuropsychiatric symptom severity, the scientists discovered that microglial activation was strongly associated with a variety of neuropsychiatric symptoms, including disturbed sleep and agitation. While levels of amyloid and tau alone were predictive of neuropsychiatric symptoms, neuroinflammation seemed to have an added effect.
Neuroinflammation was most strongly associated with caregivers or family members reporting their loved one’s rapid mood swings from calm to tears or anger, one of the common symptoms of the disease. Individuals whose caregivers showed higher levels of distress when caring for them had greater levels of brain inflammation. Taken together, the study adds to the growing evidence of the role of brain inflammation in the early stages of the disease progression, when symptoms like excess irritability tend to emerge. It also suggests that clinical trials targeting neuroinflammation as a preventive therapy for Alzheimer’s could track neuropsychiatric symptoms as one way of measuring the treatment’s effectiveness. Conversely, drugs specifically targeting neuroinflammation could potentially help reduce neuropsychiatric symptom severity and alleviate some of the psychological burden experienced by caregivers, thus improving patient support.
mRNA Quality Control in the Aging of Nematode Worms
https://www.fightaging.org/archives/2023/12/mrna-quality-control-in-the-aging-of-nematode-worms/
The nematode worm species Caenorhabditis elegans widely used in the laboratory is far removed from human biochemistry, but nonetheless there is much that can be learned about cellular mechanisms relevant to the aging of mammals. Here researchers review what is known of the role of messenger RNA (mRNA) quality control mechanisms in the aging of nematodes. mRNA is produced from gene sequences in the process of transcription, but every operation in the cell is subject to some level of error and happenstance damage to molecular structure. Thus quality control systems must exist to ensure that broken mRNA molecules do not lead to harmful outcomes, such as the production of broken, toxic proteins.
Aging is accompanied by the gradual decline in cellular and organismal fitness. At the macromolecular level, impaired protein homeostasis (proteostasis) and genome integrity are key features of aging. The age-dependent deteriorative changes are interconnected with each other to decrease the lifespan and increase the incidence of age-associated diseases, which eventually lead to death. Similar to other species, C. elegans exhibits age-associated changes such as the reduction in genome stability, proteostasis, lipid homeostasis, and immunity. Recent studies have indicated that RNA quality also declines during aging in C. elegans.
Eukaryotes are equipped with homeostatic systems that are crucial for the maintenance of mRNA quality, which is regulated by diverse surveillance pathways. Misprocessed mRNAs need to be eliminated by these RNA surveillance pathways. Nonsense-mediated mRNA decay (NMD), no-go decay, nonstop decay, and ribosome-associated quality control (RQC) are crucial for mRNA and protein quality control. mRNA splicing, which is a major pre-mRNA processing event in eukaryotes, selects and joins exons that are separated by introns, thus enabling diverse gene expression. Changes in splicing occur during aging and may reflect the deteriorated transcriptome quality. Abnormal mRNA splicing underlies the generation of aberrant transcripts that disrupts the proteostasis by producing truncated proteins and causing ribosome stalling, followed by ribosome collision.
Here we review recent studies that report on the key functions of various factors that regulate mRNA surveillance and splicing in the longevity and aging of C. elegans. Our review provides crucial information regarding the conserved functions of mRNA quality control in aging, which may be potentially utilized as therapeutic targets of aging and age-associated diseases in humans.
Muscle TFEB Overexpression Slows Cognitive Aging in Mice
https://www.fightaging.org/archives/2023/12/muscle-tfeb-overexpression-slows-cognitive-aging-in-mice/
Muscle tissue is metabolically active, and affects the operation of other organs. At this time, a good map of the important signals that pass between muscle and other tissues has yet to be created. Maintenance of muscle mass and function in later life clearly produces a more systemic benefit than simply postponing weakness and frailty, but the details of the biochemistry are not well understood. Thus researchers can perform muscle-specific interventions in animal models, such as the one noted here, show a slowing of cognitive aging to result from that intervention, but not have a good grasp of how exactly how the altered muscle tissue influences the brain in this case.
Over the last decade, growing evidence has suggested that the periphery contributes to the etiology of age-associated neurodegenerative diseases. Manipulation of skeletal muscle protein quality control pathways protects against the accumulation of aggregation-prone disease proteins in the invertebrate brain and retina. The mechanisms responsible for these benefits remain poorly understood, some of these effects are mediated by secreted factors that communicate metabolic and inflammatory signals between tissues. Although the source and identity of these neuroprotective circulating cytokines are unclear, several are known to be secreted from skeletal muscle, an unconventional endocrine organ that secretes a myriad of bioactive factors that induce metabolic changes in distant tissues such as liver, adipose tissue, and the central nervous system (CNS).
Skeletal muscle metabolism is regulated in part by transcription factor E-B (TFEB), a master regulator of the lysosomal-to-nucleus signaling that integrates cellular metabolism and lysosomal function. TFEB expression and function are strongly induced in skeletal muscle in response to interventions with neuroprotective effects against aging and neurodegenerative disease, including low nutrient conditions and exercise. TFEB controls muscle metabolic flexibility during exercise, inducing the expression of genes involved in mitochondrial biogenesis, fatty acid oxidation, and oxidative phosphorylation.
Here, we report the generation of a transgenic mouse with enhanced muscle metabolism via lifelong overexpression of TFEB. The resulting enhanced TFEB signaling protects against the onset of age-associated mitochondrial dysfunction in aging skeletal muscle. Overexpression of TFEB in skeletal muscle significantly reduces hippocampal accumulation of neuropathological hallmarks and reduces neuroinflammation in a mouse model of tauopathy, despite no exogenous activation of the transgene in the CNS. Muscle TFEB overexpression ameliorates proteotoxicity, reduces neuroinflammation, and promotes transcriptional remodeling of the “healthy” aged CNS, preserving cognitive performance in aging mice. Our results implicate maintenance of skeletal muscle function in regulating mammalian CNS health, and suggest that skeletal muscle-originating factors may act as therapeutic targets against age-associated neurodegenerative diseases.
Lower Mitochondrial Copy Number Correlates with Risk of Age-Related Macular Degeneration
https://www.fightaging.org/archives/2023/12/lower-mitochondrial-copy-number-correlates-with-risk-of-age-related-macular-degeneration/
Lower mitochondrial copy number, meaning fewer copies of mitochondrial DNA and thus presumably fewer mitochondria in a cell, is here shown to correlate with the presence of age-related macular degeneration in older individuals. Mitochondrial copy number is one approach to measuring the degree of mitochondrial dysfunction present in tissues. In the study here, it is assessed in blood samples, and is thus a measure of the health of immune cells, the degree to which they are impacted by processes of aging. Many aspects of aging tend to correlate with one another, as aging emerges from a web of various forms of damage and dysfunction that all influence one another, so one can’t draw conclusions about the degree to which mitochondrial dysfunction contributes to the development of age-related macular degeneration based on this data.
Mitochondrial dysfunction is a common occurrence in the aging process and is observed in diseases such as age-related macular degeneration (AMD). Increased levels of reactive oxygen species lead to damaged mitochondrial DNA (mtDNA), resulting in dysfunctional mitochondria, and, consequently, mtDNA causes further harm in the retinal tissue. However, it is unclear whether the effects are locally restricted to the high-energy-demanding retinal pigment epithelium or are also systematically present. Therefore, we measured mtDNA copy number (mtDNA-CN) in peripheral blood using a qPCR approach in elderly participants with and without AMD from the AugUR study (n = 2,262).
We found significantly lower mtDNA-CN in the blood of participants with early (n = 453) and late (n = 170) AMD compared to AMD-free participants (n = 1630). In regression analyses, we found lower mtDNA-CN to be associated with late AMD when compared with AMD-free participants. Each reduction of mtDNA-CN by one standard deviation increased the risk for late AMD by 24%. This association was most pronounced in geographic atrophy (odds ratio = 1.76), which has limited treatment options. These findings provide new insights into the relationship between mtDNA-CN in blood and AMD, suggesting that it may serve as a more accessible biomarker than mtDNA-CN in the retina.
Towards Drugs to Treat Sarcopenia
https://www.fightaging.org/archives/2023/12/towards-drugs-to-treat-sarcopenia/
Here, researchers review present efforts to develop drugs to treat sarcopenia, the age-related loss of muscle mass and strength that occurs in every individual, leading to eventual frailty. As a snapshot of the research and development community, it is representative of efforts across age-related disease generally, in that the primary focus falls on more easily developed options that cannot possibly produce results larger than those resulting from exercise, particular resistance exercise. This is the unfortunate outcome of the present medical regulatory system, in which the costs of regulatory approval are made so high that concerns and incentives surrounding cost outweigh all other goals.
Sarcopenia is a challenging disease for drug development, and there is currently no clinically approved therapeutic. Outcomes in clinical trials depend on functional gains in muscle performance, rather than just increases in mass, while also being well tolerated with low side effects. Sarcopenia is also a complex multifactorial disorder, and the underlying mechanisms are not fully understood. This review focused on pre-clinical drug development for sarcopenia. Due to the lack of approved therapeutics and a large projected market value, there are a large number and variety of different compounds and target pathways/cellular mechanisms under investigation.
A large proportion of current research is focusing on natural compounds and extracts, due to their characterized biological activity and advantages for further drug development. Much research effort is also focusing on the role of non-coding RNAs in sarcopenia progression, which can provide targets for small molecules currently under development for inhibiting non-coding RNA biogenesis. A number of type 2 diabetes drugs, such as SGLT2 inhibitors, DPP-IV inhibitors, and GLP-1 analogs, are also being investigated for their effects on skeletal muscle mass in type 2 diabetes patients and animal models. It will be important to consider whether these drugs can also be effective in the context of pre-diabetes or normoglycemia.
Mitochondria have a pivotal role in maintaining muscle function and are known to become dysfunctional in aging. Mitochondria-targeting drugs also hold great promise for treating sarcopenia and may utilize recent advances in mitochondria drug delivery systems. Drug repositioning strategies are also providing clinically validated candidates with known pharmacokinetics in humans. These previously characterized drugs can also provide new insights into the molecular pathways regulating skeletal muscle atrophy. A wider adoption of cell-based screening systems, based on known master regulatory genes, such as PGC-1α, could accelerate throughput and increase the number of hits for further analysis. Overall, much effort is being focused on identifying drug candidates with promising pre-clinical therapeutic activity in sarcopenia models, which raises the probability of successful drug development for this debilitating and increasingly prevalent disease.
MITF in the Regulation of Schwann Cell Nerve Repair Activity
https://www.fightaging.org/archives/2023/12/mitf-in-the-regulation-of-schwann-cell-nerve-repair-activity/
The peripheral nervous system is far more capable of self-repair than the central nervous system. Nonetheless, nerve damage typically results in far less functional regeneration than is the case for other tissues. The research community is thus interested in finding ways to enhance existing repair processes. Here, researchers investigate a portion of the regulatory mechanisms that control the activity of Schwann cells in nerve repair, in search of targets for drug development programs aimed at enhancing regeneration of nerve damage, both in the peripheral nervous system, and also potentially in the central nervous system.
The peripheral nervous system is made up of all the nerves that branch out from the brain and spinal cord to give us sensation throughout our bodies. There are many cell types in peripheral nerves, here researchers focus on understanding neurons, which transmit information throughout the nervous system, and Schwann cells, which protect healthy neurons and repair damaged ones. The peripheral nervous system’s ability to repair damage is remarkable considering that the central nervous system – made up of the brain and spinal cord – is not able to repair damage. Yet, the mechanisms that orchestrate this feat have remained poorly understood.
To unravel how Schwann cells differentiate to begin repairing peripheral nerve damage, the researchers looked at mouse models of Charcot Marie Tooth disease (CMT), a type of hereditary neuropathy. In mice with CMT, the researchers noticed that the Schwann cells completing repairs had high levels of Mitf in their nuclei – where the genetic instructions for how to be a Schwann cell and how to conduct repairs are stored. Upon investigation of this relationship between Mitf and Schwann cells, they found that Mitf was in the cytoplasm of Schwann cells until sensing neuronal damage. Damage then prompted Mitf to relocate from the cytoplasm of the cell to the nucleus, where it would direct the Schwann cell to make repairs.
To validate the importance of Mitf in creating repair Schwann cells, the researchers removed Mitf altogether. In cases of both trauma and CMT, nerve repair was arrested in the absence of Mitf – demonstrating that Mitf is required for peripheral nerve repair and regeneration. “Harnessing Schwann cell repair programs has great potential in treating chronic diseases. It’s possible that with targeted therapeutics, we can prompt more Schwann cells to repair peripheral nerve damage and push those repairs to completion in chronic cases. Furthermore, now that we have a better grasp on the repair mechanisms, we can see if it’s possible to initiate repairs in the brain stem and spinal cord, too.”
Reviewing the Role of Cellular Senescence in Pulmonary Fibrosis
https://www.fightaging.org/archives/2023/12/reviewing-the-role-of-cellular-senescence-in-pulmonary-fibrosis/
The first small human clinical trial of the senolytic therapy of dasatinib and quercetin targeted idiopathic pulmonary fibrosis, showing some benefit to patients. Later trials for kidney disease demonstrated that this treatment does remove a fraction of lingering senescent cells in human tissues in much the same way as it does in mice. Senescent cells accumulate with age in tissues throughout the body, the burden of these cells resulting from a growing gap between pace of creation and pace of clearance by the immune system. Researchers are coming to see a prominent role for senescent cells in all fibrotic conditions, in which excess extracellular matrix is produced, disrupting tissue structure and function. Compelling evidence in animal studies demonstrates reversal of fibrosis following senolytic treatment, a goal that is presently hard to achieve for human patients using existing interventions, those presently widely available in the clinic.
Pulmonary fibrosis (PF) is a chronic, progressive, devastating, and irreversible interstitial lung disease, with a median survival of 2 to 3 years after diagnosis. The present comprehension of the pathogenesis of PF entails the repetitive injury of alveolar epithelial cells (AECs) due to various risk factors, such as environmental exposure, viral infections, genetic predisposition, oxidative stress, and immunological factors. This injury subsequently results in the abnormal activation of AECs and dysregulated epithelial repair processes. The dysregulated epithelial cell secretes multiple cytokines and growth factors and interacts with endothelial, mesenchymal, and immune cells via multiple signaling mechanisms to trigger fibroblast and myofibroblast activation and promote extracellular matrix deposition, ultimately leading to the destruction of lung function, diminished exercise tolerance, and a decreased quality of life.
The existing epidemiological data from various data sources indicate that the average age of patients with PF is estimated to be over 65 years, and the incidence increases with age. Furthermore, individuals aged 70 and above have a risk of developing PF that is seven times higher than those in their 40s. Therefore, PF is now considered an age-related lung disease. Among the hallmarks of aging, cellular senescence serves as the primary driver behind tissue and organ aging, as well as an independent risk factor for PF progression. Age-related disturbances were increasingly observed in epithelial cells and fibroblasts in PF lungs compared to age-matched cells in normal lungs. Physiologically, alveolar epithelial type II (ATII) cells, serving as progenitor cells of the alveoli, differentiate into alveolar type 1 (ATI) cells in response to injury. Utilizing organoid cultures, single-cell transcriptomics, and lineage tracing, it has been discovered that ATII cells differentiate into ATI cells and acquire a transitional state known as pre-alveolar type 1 cell during the process of maturation. This transitional state exhibits regulation by TP53 signaling, making it susceptible to DNA damage and undergoing transient senescence.
However, there are at least two harmful consequences of persistent senescence. On the one hand, telomere wear and mitochondrial dysfunction lead to permanent cell-cycle arrest, which in turn causes stem cell/progenitor cell-renewal dysfunction and the loss of self-repair and regeneration abilities. On the other hand, senescent cells produce pro-inflammatory, pro-fibrotic, and stroma-remodeling cytokines such as IL-6, TGF-β, and several matrix metalloproteinases collectively known as the senescence-associated secretory phenotype (SASP), which can activate myofibroblast and scar formation. In fact, some components of SASP appear to enhance the growth arrest of exposed adjacent cells in a paracrine manner, further driving senescence, leading to low-grade chronic inflammation, and increasing susceptibility to pulmonary fibrosis.
A comprehensive understanding of how senescence promotes the occurrence and progression of PF can provide new insights into the further treatment of age-related diseases. This review presents compelling recent evidence indicating that cellular senescence is a significant driving factor in age-related lung diseases such as PF. It systematically summarizes the causes of cellular senescence in PF and the signaling pathways regulating different types of cellular senescence and also provides potential therapeutic strategies for targeting cellular senescence to improve PF. These strategies include targeting the clearance of senescent cells, intervening in senescence-related signaling pathways, and inhibiting the secretion of SASP.
A Twin Study to Assess Short Term Cardiometabolic Health Benefits of a Vegan Diet
https://www.fightaging.org/archives/2023/12/a-twin-study-to-assess-short-term-cardiometabolic-health-benefits-of-a-vegan-diet/
If you’re familiar with discussion of veganism as a lifestyle choice, nothing in this material will all that surprising. Vegans tend towards lower calorie intake and the benefits resulting from that, and that may be the dominant effect when looking at commonly measured health metrics in vegan study participants. It would be interesting to see more comparison studies in which the vegans were held to the same calorie intake as the omnivore control participants, but, alas, that is logistically harder and thus not the approach chosen by most study organizers.
Although it’s well-known that eating less meat improves cardiovascular health, diet studies are often hampered by factors such as genetic differences, upbringing and lifestyle choices. By studying identical twins, however, the researchers were able to control for genetics and limit the other factors, as the twins grew up in the same households and reported similar lifestyles. The trial, conducted from May to July 2022, consisted of 22 pairs of identical twins for a total of 44 participants. The study authors selected healthy participants without cardiovascular disease from the Stanford Twin Registry – a database of fraternal and identical twins who have agreed to participate in research studies – and matched one twin from each pair with either a vegan or omnivore diet.
The authors found the most improvement over the first four weeks of the diet change. The participants with a vegan diet had significantly lower low-density lipoprotein cholesterol (LDL-C) levels, insulin, and body weight – all of which are associated with improved cardiovascular health – than the omnivore participants. At three time points – at the beginning of the trial, at four weeks and at eight weeks – researchers weighed the participants and drew their blood. The average baseline LDL-C level for the vegans was 110.7 mg/dL and 118.5 mg/dL for the omnivore participants; it dropped to 95.5 for vegans and 116.1 for omnivores at the end of the study. The optimal healthy LDL-C level is less than 100.
Because the participants already had healthy LDL-C levels, there was less room for improvement. Researchers speculated that participants who had higher baseline levels would show greater change. The vegan participants also showed about a 20% drop in fasting insulin – higher insulin level is a risk factor for developing diabetes. The vegans also lost an average of 4.2 more pounds than the omnivores.
Clumps of Cells as a Novel Basis for Regenerative Medicine
https://www.fightaging.org/archives/2023/12/clumps-of-cells-as-a-novel-basis-for-regenerative-medicine/
Researchers here note an interesting project, the production of self-assembling, mobile clumps of cells propelled by cilia, formed from lung epithelium. These mobile bodies can encourage growth in nerve cells, at least in vitro. How exactly that happens remains to be determined, but the usual mechanism is via release of pro-growth factors, either directly, or encapsulated in extracellular vesicles. Whether this is a useful basis for future regenerative therapies remains to be seen; one might imagine concerns attending the introduction of large numbers of these epithelial cell bodies into other tissues. The full paper is nonetheless an interesting read.
Researchers had previously developed tiny robots using clumps of embryonic frog cells. But the medical applications of these ‘xenobots’ were limited, because they weren’t derived from human cells and because they had to be manually carved into the desired shape. The researchers have now developed self-assembling ‘anthrobots’ made of human cells and are investigating their therapeutic potential using human tissue grown in the laboratory.
The researchers grew spheroids of human tracheal skin cells in a gel for two weeks, before removing the clusters and growing them for one week in a less viscous solution. This caused tiny hairs on the cells called cilia to move to the outside of the spheroids instead of the inside. These cilia acted as oars, and the researchers found that the resulting anthrobots – each containing a few hundred cells – often swam in one of several patterns. Some swam in straight lines, others swam in circles or arcs, and some moved chaotically.
To test the anthrobots’ therapeutic potential, researchers placed several into a small dish. There, the anthrobots fused together to form a ‘superbot’, which the researchers placed on a layer of neural tissue that had been scratched. Within three days, the sheet of neurons had completely healed under the superbot. This was surprising because the anthrobot cells were able to perform this repair function without requiring any genetic modification. Going forward, researchers think anthrobots made from a person’s own tissue could be used to clear arteries, break up mucus or deliver drugs, with or without genetic engineering.