Babies in WA will soon be immunised against RSV – but not with a vaccine

This week, Western Australia announced a state government-funded immunisation program against respiratory syncytial virus (RSV). It’s the first Australian state or territory to do so.
All babies under eight months old and those aged eight to 19 months at increased risk of severe RSV infection will be eligible for the immunisation in WA this year.
RSV can cause serious illness in children, and news headlines have welcomed WA’s impending rollout of “vaccinations” against the virus.
But this immunisation differs from other routine childhood vaccines.
Why is RSV important?
RSV is the most common cause of respiratory infection in young children. By the age of two, almost all children show evidence they’ve been exposed to the virus.
Estimates suggest 2-3% of infants are hospitalised with RSV with infection involving the airways and lungs. Infants under three months are at highest risk. RSV can also have long-lasting effects on children – there’s a well-established link between RSV and subsequent wheezing illnesses and asthma.
RSV can also be a problem for the elderly and people with underlying health conditions such as those with weakened immune systems.
Read more:
An RSV vaccine has been approved for people over 60. But what about young children?
How do we protect children against RSV?
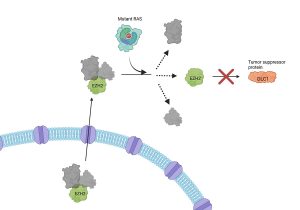
Antibodies are a key part of the immune system that protect people against many viral infections, including RSV. They’re usually generated in response to infection or a vaccine, and work by attaching to proteins on the surface of RSV, therefore preventing the virus from invading the cells that line the airways and lungs.
The problem in newborn babies (who are at the highest risk of severe RSV infection) is that previous vaccines have not generated sufficient antibodies to provide protection.
So, two strategies have been developed to protect young children against RSV. These strategies are both referred to as passive immunisation, because children receive protective antibodies from outside the body. This is different to active immunisation where we give a child a vaccine so they can generate their own antibodies.
Ground Picture/Shutterstock
Vaccination in pregnancy
One way to deliver passive immunity to young infants is by vaccinating their mothers during pregnancy. Maternal immunisation has been shown to be effective at protecting infants from other infections, including influenza, whooping cough (pertussis), tetanus and COVID.
By delivering a single RSV vaccine to pregnant women, antibodies are generated by the mother and transported across the placenta, providing passive immunity and protection to the baby for around the first six months of life. In a clinical trial, giving an RSV vaccine in late pregnancy reduced RSV in young infants by approximately 70%. But RSV vaccines for pregnant women are not yet available in Australia.
Read more:
RSV is everywhere right now. What parents need to know about respiratory syncytial virus
What are monoclonal antibodies?
The other passive immunisation strategy relies on manufactured long-acting antibodies (known as “monoclonal antibodies”), which can be delivered by injection to young children.
This is what will be offered in WA. Nirsevimab (also known as Beyfortus) is a long-acting antibody that Australia’s Therapeutic Goods Administration (TGA) approved in November 2023.
Nirsevimab binds specifically to RSV and remains in the body for several months after injection. In a key clinical trial nirsevimab was shown to reduce RSV infections by about 75% for up to five months.
Several European countries have recently implemented infant programs with nirsevimab and are reporting significantly lower RSV hospitalisation rates in babies.

Allen Mercer/Shutterstock
Antibody therapies in various forms have been used for more than a century for the prevention and treatment of a range of conditions, dating from “serotherapy” for tetanus, diphtheria and snake bite in the late 1800s.
Licensed antibody products are rigorously tested in clinical trials and through post-marketing surveillance to ensure their safety.
For nirsevimab specifically, the clinical trial mentioned above included over 1,400 infants. Adverse events were reported at similar rates in the nirsevimab and placebo groups, and no serious adverse events relating to treatment were reported. No significant safety concerns have been identified in the real-world rollout in the northern hemisphere either.
When does RSV occur?
RSV usually takes hold just before the flu season in southern states, and circulates year-round in tropical areas. While influenza almost disappeared during the COVID pandemic, there were ongoing cases of RSV, albeit with a disruption to the normal seasonal pattern.
Since 2022, RSV has resumed its normal seasonal pattern. The WA government says the immunisations will be available from April, which is timely in anticipation of the 2024 season.
Read more:
RSV is a common winter illness in children. Why did it see a summer surge in Australia this year?
What about other states and territories?
Free access to an immunisation against RSV should significantly benefit young children and families in WA, keeping children out of hospital this winter.
Whether other states will follow WA’s lead is uncertain at this stage, and we don’t yet know whether nirsevimab will in time become part of the National Immunisation Program, meaning it would be available for free nation-wide.
Ensuring equitable access, particularly for those at greatest risk of severe RSV infection, must be prioritised to ensure maximum benefit for all children and families.
Nirsevimab is likely to be the first of many tools to prevent RSV in children. A maternal RSV vaccine is currently under assessment by the TGA and Pharmaceutical Benefits Advisory Committee (PBAC). A vaccine for older Australians, Arexvy, is registered and is also being assessed by the PBAC, with additional vaccines expected to be available in the future.
These developments highlight the future of RSV prevention and also the significant potential for monoclonal antibodies to play a greater role in preventing infections as part of public health programs.