Interview with Stefany Shaheen: Revolutionizing diabetes care through cell therapies
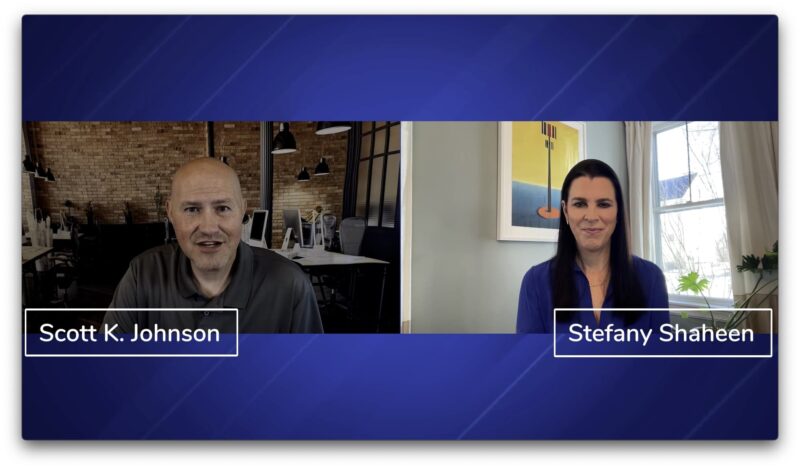
[00:00:00] Scott K. Johnson: I’m excited to introduce Stefany Shaheen, Chief Strategy Officer of Advanced Regenerative Manufacturing Institute, or ARMI. And BioFab USA, a program of ARMI. Stefany’s background is remarkable. She has four children, and her eldest daughter, Elle, lives with diabetes. She graduated from MIT’s Sloan School of Management and Harvard’s Kennedy School of Government.
[00:00:38] Scott K. Johnson: She is a New York Times best-selling author for her book ‘Elle and Coach, Diabetes, The Fight for My Daughter’s Life and The Dog Who Changed Everything’ (affiliate link). She is the President and Co-Founder of Good Measures, LLC. She serves on the President’s Council on Sports, Fitness, and Nutrition and recently completed her term serving as Police Commissioner in Portsmouth, NH, where she also served on the City Council.
[00:01:06] Scott K. Johnson: Stefany served on the Board of Trustees for the Joslin Diabetes Center, and was the National Chair of JDRF’s Children’s Congress, and served on the Foundation’s Advocacy Committee. Stefany, even with all that I’ve mentioned, I feel like I’ve only just scratched the surface of your story. Is there anything that I missed that you’d like people to know?
[00:01:28] Stefany Shaheen: I think you covered all the highlights. I’m grateful to join you today, Scott and I look forward to our conversation.
[00:01:35] Scott K. Johnson: My pleasure. So today we’re going to talk about the transformational potential of cell therapies for people living with diabetes. I’m not very familiar with what that means.
[00:01:48] Scott K. Johnson: Can you tell us more about it? And what is cell therapy for type 1 diabetes?
[00:01:53] Stefany Shaheen: Sure. Well, and maybe I’ll start by just sharing, you know, I think for anyone who’s been touched by diabetes, you can imagine and remember what life felt like B. D., which is what we say in our family before diabetes, and A. D., after diabetes.
[00:02:09] Stefany Shaheen: And really, following my daughter Elle’s diagnosis when she was eight with type 1, I really think my life’s trajectory changed dramatically, and I remember she was part of a clinical trial back then led by Dr. Kevan Herold, at Yale New Haven Hospital, and I remember having a conversation with him while she was in the hospital getting a, a drug therapy that was part of a clinical trial, and I said, you know, who shares our sense of urgency about what it’s going to take to actually have a cure for type 1 diabetes?
[00:02:41] Stefany Shaheen: And the first person he mentioned was Dr. Doug Melton at Harvard Stem Cell Institute and at Harvard, who’s now at Vertex, uh, and that really, It sparked me to reach out to him way back then, 16 years ago now, and I’ve followed his work and trajectory ever since. And for those of, you know, for those listeners who don’t know, Doug Melton, is a biologist and a researcher at Harvard, tenured faculty who recently took a leave of absence to go to Vertex.
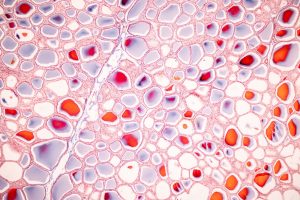
[00:03:10] Stefany Shaheen: Because Vertex licensed his intellectual property and his research really designed to develop cell therapy for people living with diabetes. So the idea is to take the insulin secreting beta cells that our bodies make if we don’t have type 1 diabetes, and those cells are what’s required to respond to sugar in the blood and to convert food into energy in the body.
[00:03:35] Stefany Shaheen: And so synthetic insulin replaces that function. But obviously, anyone who lives with having to take continuous doses of insulin recognizes it’s far from a cure. And the goal really is to replace those cells in the pancreas that people who live with type 1 don’t have. So what he discovered was that you could take a pluripotent stem cell.
[00:03:57] Stefany Shaheen: So I like to think of this like back in the day when we had floppy disks on computers and nothing was on them. Or you can think of a zip drive that doesn’t have any files stored on it. The idea of those pluripotent stem cells is that they have yet to be programmed into a specific function. So they’re not yet a blood cell or a neural cell or a beta cell, which is what people with type 1 need.
[00:04:18] Stefany Shaheen: And then he developed a mechanism through which to program that pluripotent stem cell into a beta cell. So, a cell that actually can respond to glucose in the blood can secrete insulin. And there’s been already now several people who’ve received cell transplants using the same, you know, using the approach that Dr. Melton developed through Vertex in clinical trials.
[00:04:38] Stefany Shaheen: And we’ve seen that those cells have actually resulted in a dramatic reduction in the need for synthetic insulin and in some cases, at least in one case, we know publicly, a complete elimination of the need for synthetic insulin. The promise is that we can find ways to manufacture those cells at scale and we can find ways to put them in the body safely so that one day very soon, we hope, people who are living with type 1 diabetes will not need continuous synthetic insulin to live.
[00:05:15] Scott K. Johnson: I like the sound of that a lot. I mean, one of the challenges that we struggle with living with diabetes is delivering insulin into the subcutaneous tissue. It’s so different than what someone without diabetes experiences, that it really creates a lot of variables. So this sounds really, really promising.
[00:05:36] Scott K. Johnson: Can you tell us a little bit more about the current status of the potential cell therapies?
[00:05:43] Stefany Shaheen: Doug Melton was the first person to really lead the way and published a lot of the results of his research over now 20 years. So this, you know, people may just be hearing about it, but it represents years and years of work and tremendous investment and expertise on the part of the world’s really leading biologists.
[00:06:01] Stefany Shaheen: There are several others who are in the mix who are working on their own approach to how to do this. Uh, Novo Nordisk is working on a cell program. There are other smaller biotech startups working on a cell program, including Katie Digovich at Minutia. Katie also lives with type 1.
[00:06:22] Stefany Shaheen: We know, SANA Therapeutics is working on cell therapy. So there are many, many approaches to this. And I’ve just given you a few examples. People are testing everything from how do we make the cells reliably at scale? Where do we put the cells? How do we protect the cells? Because right now, you know, if you were to put a new batch of cells into my daughter’s body, her immune system would do the same thing to those cells as it’s done to the cells she used to have, right?
[00:06:49] Stefany Shaheen: So trying to figure out how do we best protect those cells? Do we encapsulate them? Do you have to take immunosuppression? Obviously, people wouldn’t subscribe to immunosuppression unless it was a last resort. So the goal is to really find a way to avoid having to have, have that be the reality.
[00:07:06] Stefany Shaheen: So there’s lots of research. I think this is actually, for anybody who’s followed scientific discovery or evolution of medical treatments. I see cell therapy, and eventually gene therapies today, the way that biologics were 30-plus years ago. We’re on the precipice of a whole host of discoveries and developments that are really going to transform the way people treat and live with chronic disease.
[00:07:34] Scott K. Johnson: Yeah, it sounds fascinating and it’s exciting to me to hear that there are so many people working on this. Can you touch on some hurdles for getting cell therapies approved?
[00:07:49] Stefany Shaheen: Absolutely. And I think this is an important area of work. There is need for more energy and attention on the regulatory side because the science is really catching up.
[00:08:02] Stefany Shaheen: The promise and the science are very, very close to one another now. It used to be we had this vision, this dream, you know, Dr. Melton’s notion that you could actually restore and replace these cells. We have to be ready to go. Can we get them reimbursed by health plans?
[00:08:35] Stefany Shaheen: How do you make the case, from a health policy standpoint, that one or two doses of cells over a person’s lifetime are a more cost-effective strategy than continuous insulin with medical devices and all the complications that come from that? That’s a public policy challenge that we really need to begin tackling now.
[00:08:55] Stefany Shaheen: But I think even more urgent is this notion of what is it going to take on the regulatory side to get cell and gene therapies approved. If you think about the evolution of the FDA. We know how to regulate drugs. We know now how to better regulate medical devices. This is a brave new world. Cell and gene therapies are new.
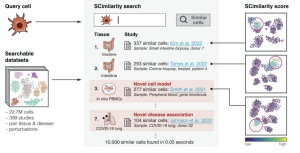
[00:09:13] Stefany Shaheen: And it’s different, you know, it’s a different construct to be wrestling with. Proving that one vial of insulin looks the same from the next to the next to the next is different than a biological material like a cell. And so that’s one of the things that ARMI is working very hard on is to develop the standards and the data analytics needed to show folks like the FDA, look, this batch of cells looks the same as the next batch of cells, and the next batch of cells.
[00:09:42] Stefany Shaheen: So they have the assurance that there are standards, that there’s ability to scale, that there’s consistency from batch to batch. And those are the kinds of things we’re really going to need in order to scale these discoveries. Yeah.
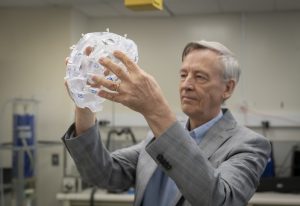
[00:09:55] Scott K. Johnson: Can we maybe dig into that a little bit more? I had the pleasure of Hearing Dean Kamen speak at Amy Tendrich’s Diabetes Mine Innovation Summit here in San Diego last November.
[00:10:08] Scott K. Johnson: And what really struck me was Dean’s focus and expertise on taking an idea and producing something, which is one kind of monster in itself, but also looking at how to do so safely and reliably, consistently, and at scale with affordability in mind and kind of growing these systems and best practices that can then kind of help launch the entire industry forward. Can you talk a little bit more about that?
[00:10:38] Stefany Shaheen: Absolutely. You know, I think that’s the power of what we’re building. We call the area where we’re building the Advanced Regenerative Manufacturing Institute, RegenValley, and the hope is to really build out the industry of regenerative manufacturing because the reality is you have incredible biology being done in labs, and you have some breakouts and breakthroughs like the work being done at Vertex.
[00:11:04] Stefany Shaheen: But many, many discoveries languish in an academic lab because there’s not a partner on the engineering side or the commercialization side to take it from the lab to, to market. And ARMI is intended to do that. It’s to bridge that divide. to combine the power of science and biology with the engineers who can then identify how we scale this affordably, and effectively. How do we demonstrate to the FDA that there’s no batch-to-batch variability, that a batch of cells that comes out on Monday is consistent with the same batch of, another batch of cells that comes out on Friday.
[00:11:40] Stefany Shaheen: That’s a whole different area of expertise than the expertise of the people developing the way to take a pluripotent stem cell and turn it into a beta cell. So that’s really what we’re doing. We’re working to translate the research of scientists like Dr. Jeffrey Millman and others
[00:11:59] Stefany Shaheen: and say, okay, they know how to do this in the lab. Now, how do we do this reliably on a manufacturing line at scale such that we can make it affordable for people and it actually can work. You know, for, for millions – not a small human clinical trial
[00:12:14] Scott K. Johnson: There’s a really great video that I’ll link in the show notes and the blog post, on the website that talks about taking these discoveries from Petri dish and Petri dish to the large scale thing.
[00:12:30] Scott K. Johnson: I really appreciated that. That expertise is something that I hadn’t thought about before. You know, the million-dollar question, right? When might people living with type 1 be able to benefit from some of these cell therapies?
[00:12:47] Stefany Shaheen: Yeah, as you know, it’s always dangerous to try to put a timeline.
[00:12:51] Stefany Shaheen: I know when Elle was diagnosed, people said, five years, you’re going to see a cure in five years. And it’s been 16 years. I never want to be part of a process that gives people false hope. But I can say, that given the acceleration in this space, given the promising results that have been demonstrated with the biology and the science, the hard part really has been – I mean, there are still hard parts – but the hard part is, how do you make a, how do you make a cell become a beta cell so that you don’t need to only have, you know, cadaver cell source or, you know, there’s been some research done from other animals. Can you translate, you know, insulin from other animals and use that in people?
[00:13:33] Stefany Shaheen: That doesn’t scale, right? So we’ve solved this source of the cell problem. And now, the act of actually scaling it and doing it reliably batch after batch after batch, that’s a very solvable problem. And we feel very confident we’re on the way to doing that reliably and having the data analytics needed for partners like the FDA to say, okay, now we can approve far more human clinical trials and really accelerate the path to getting this into people.
[00:14:04] Stefany Shaheen: So I’m hopeful. My daughter is 24.I hope that before she decides she’s ready to have a child, she’ll be able to have a cell therapy. Whether that’s a few years or, you know, 5, 6, 7, 8 years, who’s, who’s to say? But I certainly believe we’re much closer now than ever before and I can confidently say there will be a cell therapy in her lifetime. We are very close.
[00:14:31] Scott K. Johnson: Really, really exciting. I’ve lived with diabetes, it’ll be 44 years next month. And I remember the similar promises – the five years. I think that working on diabetes, it’s a very complicated problem. And as soon as you solve one layer of problems, a bunch of new layers pop up! But I continue to be excited and inspired by great people like yourself and the folks at ARMI and BioFabUSA, and all the amazing others who are continuing to work so hard on, on all of this.
[00:15:14] Scott K. Johnson: Is there anything that those of us in the diabetes community or even the general public can do to help?
[00:15:22] Stefany Shaheen: I love that question. I think there really are many ways to help. One is making sure your members of Congress appreciate the value of the special diabetes program.
[00:15:34] Stefany Shaheen: That’s funding that makes this kind of research possible on an ongoing basis and it’s critical for that funding to continue. Advocating with the FDA relative to defining a regulatory pathway that’s going to make it possible to get human clinical trials approved. And then, if you’re brave enough or bold enough or have the capacity, consider being part of a human clinical trial when the day comes that there are more clinical trials available to people in this country. I think the unfortunate reality right now is that because we haven’t carefully prescribed the regulatory pathway here, these trials are currently happening in Canada and in Australia, New Zealand.
[00:16:13] Stefany Shaheen: And I feel very strongly that those clinical trials should be happening here. The science was all developed here. They are going to be manufactured here. They’re going to be put in people here. So the idea that these clinical trials can’t happen here, I just reject outright. So I think when the time comes, being willing to participate in these trials will be important.
[00:16:34] Stefany Shaheen: And then, I think just remaining hopeful and engaged, you know? I mean, partners like the Juvenile Diabetes Research Foundation, who have been so instrumental in funding and really pushing this work forward. If you participate in a walk for JDRF, if you are part of, if you attend an annual gala for them, if you help raise money in any capacity, or volunteer to be part of a government day, those things really do matter.
[00:17:01] Stefany Shaheen: And I can say, having seen up close and personally, just how valuable the funding is that JDRF is. It’s not just the dollars, it’s also the leadership to target the monies in the best possible way to leverage those investments. I highly encourage folks, to do whatever they can to be engaged with JDRF and help raise money to support this research.
[00:17:24] Scott K. Johnson: Yeah. Wonderful. Wonderful. Well, Stefany, I know we’ve covered a lot of ground. Is there anything that you’d like to talk about that I haven’t asked about?
[00:17:36] Stefany Shaheen: One of the things that I’ve recently heard that I think is a really powerful construct, and it might be useful for people who live with type 1 to think of it this way, you know, for so long, when we think about diabetes, we treat it like a metabolic disorder.
[00:17:51] Stefany Shaheen: And so, as long as people think of it as a metabolic disorder, the notion of having insulin – It feels almost curative, right? Your metabolic system needs insulin; you don’t have insulin, so we’re going to replace the insulin. But the reality is that type 1 is an autoimmune disorder. It’s an autoimmune disease.
[00:18:08] Stefany Shaheen: And if you start to really think about it in that way, it changes how you approach the care and treatment of the disease. So everything from screening to early screening for people identifying whether you’re genetically predisposed to ultimately developing the disease. Then, having treatment before you actually have full-onset diabetes.
[00:18:30] Stefany Shaheen: Thinking about it in stages instead of with or without. Then you start to think about these curative cell therapies and, you know, maybe it isn’t like a switch where one day you have to take continuous insulin either with injections or a pump. And the next day you don’t. Maybe there’s some incremental therapies that can happen that get you to full insulin independence or synthetic insulin independence.
[00:18:52] Stefany Shaheen: So, I’ve listened to researchers who are starting to think about it in this way and hopefully the regulators will start, will start to think about it in this way. And then, eventually, health plans will start to think about it in this way. So we can do things like, I mean, no person should ever die because they weren’t diagnosed.
[00:19:09] Stefany Shaheen: No person, because they just didn’t know the science. We should know the science. We should know a person’s at risk, because we now have ways of helping stave off onset. We have the approval of tzield – this drug that allows for a delay in onset. And so I hope that as we, as an advocacy community, for people who live with the disease can start to think about it.
[00:19:34] Stefany Shaheen: And it’s really this frame of, no, it’s really an autoimmune disease. We treat it like it’s a metabolic disorder, but it’s an autoimmune disease, and let’s tackle it that way. Because I do think ultimately that will mean people are healthier and safer long term.
[00:19:48] Scott K. Johnson: Yeah, absolutely. I also like your idea and approach of this stepwise and incremental approach.
[00:19:55] Scott K. Johnson: And it makes me think, you know, of how many changes I’ve seen in my lifetime with diabetes, moving from urine testing to home blood sugar testing to CGMs and then automated insulin delivery systems. Life is so much better for me today than it was 40 years ago. I don’t want that to slow down.
[00:20:19] Scott K. Johnson: I hope that it continues to get better as time, as time goes on until eventually I reach a point where I don’t have to think about my diabetes at all. So I think that incremental approach, there’s a lot of value in that. So thank you for bringing that up.
[00:20:32] Stefany Shaheen: For sure, and I just, maybe this is an appropriate place to close. I thought a lot about Supreme Court Justice Sonia Sotomayor, who described during Children’s Congress her reality of, she said she could still picture the little stool she stood on as a child to boil her needles to sterilize them, you know, her little glass syringes, and talked about how far things have come. And when I think about my own daughter’s trajectory in the 16 years she’s lived with this disease. It started with multiple daily injections and finger sticks, and now she has a closed-loop system, and she can walk out of the house with just her phone. She wears an Omnipod and a Dexcom CGM, and it’s controlled by her phone. Yet the reality is that she still lives with the same risks, and as you point out, the number of decisions and energy it requires to manage this disease.
[00:21:27] Stefany Shaheen: And so we’ve got to keep pushing for even better curative therapies that are going to totally transform the way people currently have to live with type 1. I’m privileged to be on this journey to help push us in this direction. I’m grateful for the conversation today, and for everything your listeners will do to help us get one step closer.
[00:21:47] Scott K. Johnson: Absolutely. I’m privileged to host the conversation and just thank you so much for all the work that you’re doing at ARMI and BioFabUSA, but also just everything else you’re doing. As mentioned in the intro, you are incredibly busy and involved in many, many things that do so much good for others. So thank you, Stefany, for that.
[00:22:11] Stefany Shaheen: Thank you, Scott. I really appreciate our conversation today.