The molecular underpinnings by which traumatic brain injury increases Alzheimer’s disease risk
Researchers found that traumatic brain injury increases synaptic dysfunction and cognitive impairments linked to developing Alzheimer’s disease.
A recent study in Acta Neuropathologica investigated the relationship between tau protein and BCL2-associated athanogene 3 (BAG3) and its possible role in traumatic brain injury (TBI) pathology.
Background
Traumatic brain injuries are a leading cause of mortality and disability in the United States. Growing evidence suggests that TBI in early or middle age increases the likelihood of acquiring Alzheimer’s disease (AD) and related dementia (ADRD). However, the biological pathways behind TBI-inflicted Alzheimer’s disease-like disease and cognitive impairments are unknown.
Previous investigations have shown that BAG3 modulates tau protein clearance. BAG3 enhances autophagy, which presumably reduces protein aggregation. Neuronal BAG3 deficiency exacerbates pathogenic tau protein accumulation, whereas overexpression reduces tau formation.
In Alzheimer’s disease, BAG3 levels decrease in excitatory neurons while increasing in astrocytes. BAG3 in astrocytes protects against alpha-synuclein and tau-related disorders. Thus, BAG3 regulates the cellular sensitivity to tau-related pathology in Alzheimer’s disease.
About the study
The present study explored BAG3’s involvement in TBI-related pathology, including tau phosphorylation, synaptic dysfunction, memory loss, and gliosis.
The researchers used wild-type and humanized tau knockin (hTKI) mice for animal experiments. To corroborate the pathological profiles of TBI found in animal models, they investigated the pathological profiles of postmortem brains of humans with TBI history or without. They obtained human brain tissue from the Banner Health Institute Brain Bank.
The control cases had the lowest National Institute on Aging-Alzheimer’s Association (NIA-AA) scores. TBI subjects without a confirmed AD diagnosis exhibited NIA-AA levels ranging from medium to high. Patients with a confirmed AD diagnosis with or without TBI exhibited high NIA-AA scores. The scientists chose the inferior parietal lobe (IPL) of the human brain for investigation since it is one of the areas most impacted by TBI.
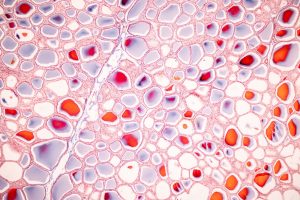
Proteins isolated from mouse and human brains underwent immunofluorescence (IF) analysis. Since human fresh frozen sections include lipofuscin, an autofluorescent material that can skew IF findings, researchers suppressed autofluorescence using light-emitting diode (LED) arrays. Western blot (WB) assays evaluated the protein fractions produced by electrophoresis.
Researchers used human embryonic kidney 293 (HEK293) cells to examine synaptic integrity following TBI and autophagy. Since synaptic disruption relates to cognitive issues, they measured cognitive function. They caused TBI using controlled cortical impact (CCI). They conducted behavioral assessments like the Y-maze, open-field test, and Morris water maze. The Y-maze test evaluated spatial working memory. The open-field test measured exploratory and locomotor activity changes.
The Morris Water Maze exam assessed spatial learning and memory. Furthermore, researchers investigated whether boosting BAG3 levels in neurons may reduce TBI-induced pathology and prevent synaptic dysfunction in hTKI mice. They overexpressed BAG3 in hippocampus neurons using stereotaxic unilateral injections.
Results
TBI caused by cortical impact lowered BAG3 expression in oligodendrocytes (OLG) and excitatory neurons, resulting in tau buildup. In wild-type and hTKI animals, disrupting BAG3 homeostasis caused synaptic dysfunction, gliosis, and cognitive impairments. Reduced postsynaptic density protein 95 (PSD95) staining showed postsynaptic dysfunction. Mice performed poorly in the Y-maze test and showed changed performances in the open-field test after TBI, aligned with synaptic results.
BAG3 knockdown drastically reduced autophagic flow, but overexpression considerably boosted it in the in vitro settings. Overexpressing BAG3 in hippocampal cells reduced AD-like pathologies and cognitive impairments caused by traumatic brain injury among hTKI mice by stimulating the autophagy-lysosome pathway (ALP).
BAG3 levels rose in glial fibrillary acidic protein (GFAP)-expressing astrocytes. The results suggest that astrocytes may upregulate BAG3 as a compensatory strategy to defend themselves against tau accumulation or aid in clearing tau aggregates.
The number of GFAP-positive astrocytes and Ionized Calcium-Binding Adapter Molecule 1 (IBA1)-positive microglia increased as PHF1+ tau pathology progressed. The data suggest that astrocytes and microglia increase in areas with tau disease.
Inverse correlations between BAG3 and PHF1 expression show that cells with phosphorylated tau accumulation had much lower BAG3 levels than cells without it. Thus, BAG3 loss might lead to tau protein buildup in oligodendrocytes following TBI or AD.
Overexpressing neuronal BAG3 may lower the burden of tau buildup and mitigate memory issues following TBI. BAG3 overexpression also improved ALP efficiency in vivo. However, neuronal BAG3 overexpression alone cannot diminish the gliosis observed after TBI. The team discovered identical alterations in human TBI cases and exaggerated findings in human AD cases with TBI.
Conclusion
The study found that TBI affects BAG3 expression in neurons, oligodendrocytes, and astrocytes, rendering cells less or more susceptible to tau buildup following TBI. BAG3 inhibits tau phosphorylation, synaptic disruption, and cognitive impairments caused by TBI via modulating the ALP pathway.
The results indicate that targeting neuronal BAG3 may be a therapeutic strategy to prevent or reduce AD-like cognitive and pathological changes caused by TBI.