Atlas of Alzheimer’s disease progression
October 29, 2024
At a Glance
- Researchers constructed an atlas of cellular changes in the brain during Alzheimer’s disease.
- The findings revealed two distinct phases of disease progression and suggest potential treatment targets.
Alzheimer’s disease (AD) features a characteristic accumulation of pathological proteins in the brain. These include amyloid beta (Aβ) plaques and tau tangles. But which specific cell types in the brain are affected has not been well-studied. To remedy this, the NIH-funded Seattle Alzheimer’s Disease Brain Cell Atlas (SEA-AD) consortium set out to produce a high-resolution atlas of the cellular and molecular changes that occur in the brain during AD.
As part of this effort, a team led by researchers at the Allen Institute and the University of Washington mapped AD-related changes in a brain region called the middle temporal gyrus. This region is involved in language, memory, and visual processing. It is thought to be a key area in the transition from early- to late-stage AD pathology. The team examined the middle temporal gyrus from the brains of 84 donors in various stages of AD. All donors were at least 65 years old when they died (average age 88 years). There were more female than male donors, consistent with the observation that AD is more common in females.
For each donor, the researchers assessed AD pathology and collected data on gene activity and epigenetic modifications—modifications to the genome that don’t affect the DNA sequence itself—in individual cells. From the pathology data, they were able to order the donors along a continuum of disease progression. They could then relate any observed cellular or molecular changes to disease progression. Cells were classified by comparing their molecular features to a reference from the NIH BRAIN Initiative®. Results appeared in Nature Neuroscience on October 14, 2024.
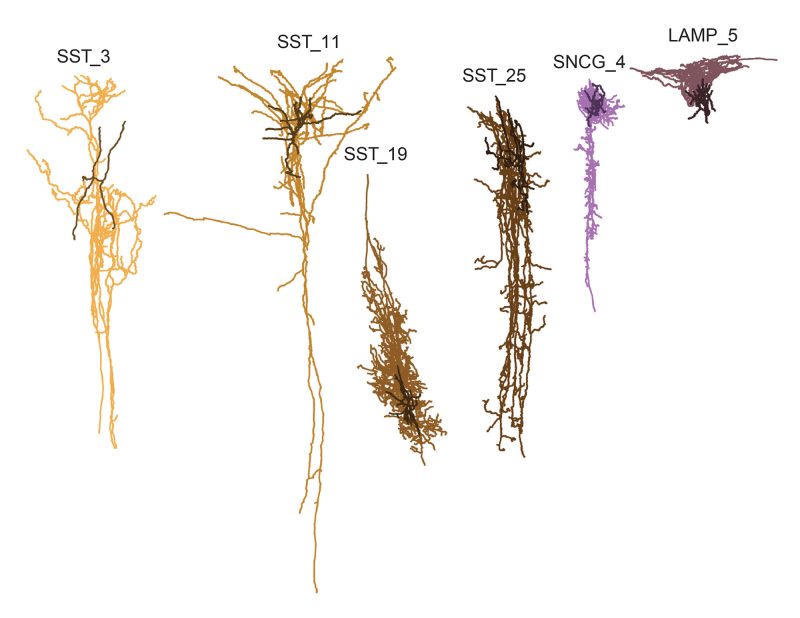
The analysis revealed two distinct phases of AD progression. In the early phase, Aβ plaques and tau tangles were sparse and grew slowly. In brain immune cells called microglia, there was increased activity in inflammatory genes. Other immune cells called astrocytes also showed signs of increased activation. There was a loss of support cells called oligodendrocytes. To compensate, those oligodendrocytes that remained ramped up their activity. Notably, numbers of a particular type of inhibitory neuron decreased. The loss of these neurons could have wide-ranging consequences for brain function.
In the later phase, the number of plaques and tangles increased exponentially. More types of neurons, both excitatory and inhibitory, began to be lost. Astrocytes and microglia remained inflammatory, while oligodendrocyte activity went down.
The team applied the same analysis to publicly available data from another ten AD studies. These comprised more than 700 donors spanning a similar range of AD stages. The results supported many of the findings from the SEA-AD data.
The findings suggest that the early loss of certain inhibitory neurons might drive later AD pathology. By identifying the earliest affected neurons, the findings highlight new potential treatment targets.
“You could say that we created a pathology clock that tells not only what changes are happening in this cortical region, but when,” says lead author Dr. Mariano Gabitto of the Allen Institute. “We now have a framework to arrange the sequence of events as Alzheimer’s pathology increases over time.”
—by Brian Doctrow, Ph.D.
Related Links
References: Integrated multimodal cell atlas of Alzheimer’s disease. Gabitto MI, Travaglini KJ, Rachleff VM, Kaplan ES, Long B, Ariza J, Ding Y, Mahoney JT, Dee N, Goldy J, Melief EJ, Agrawal A, Kana O, Zhen X, Barlow ST, Brouner K, Campos J, Campos J, Carr AJ, Casper T, Chakrabarty R, Clark M, Cool J, Dalley R, Darvas M, Ding SL, Dolbeare T, Egdorf T, Esposito L, Ferrer R, Fleckenstein LE, Gala R, Gary A, Gelfand E, Gloe J, Guilford N, Guzman J, Hirschstein D, Ho W, Hupp M, Jarsky T, Johansen N, Kalmbach BE, Keene LM, Khawand S, Kilgore MD, Kirkland A, Kunst M, Lee BR, Leytze M, Mac Donald CL, Malone J, Maltzer Z, Martin N, McCue R, McMillen D, Mena G, Meyerdierks E, Meyers KP, Mollenkopf T, Montine M, Nolan AL, Nyhus JK, Olsen PA, Pacleb M, Pagan CM, Peña N, Pham T, Pom CA, Postupna N, Rimorin C, Ruiz A, Saldi GA, Schantz AM, Shapovalova NV, Sorensen SA, Staats B, Sullivan M, Sunkin SM, Thompson C, Tieu M, Ting JT, Torkelson A, Tran T, Valera Cuevas NJ, Walling-Bell S, Wang MQ, Waters J, Wilson AM, Xiao M, Haynor D, Gatto NM, Jayadev S, Mufti S, Ng L, Mukherjee S, Crane PK, Latimer CS, Levi BP, Smith KA, Close JL, Miller JA, Hodge RD, Larson EB, Grabowski TJ, Hawrylycz M, Keene CD, Lein ES. Nat Neurosci. 2024 Oct 14. doi: 10.1038/s41593-024-01774-5. Online ahead of print. PMID: 39402379.
Funding: NIH’s National Institute on Aging (NIA), National Institute of Neurological Disorders and Stroke (NINDS), and National Institute of Mental Health (NIMH); University of Washington Nancy and Buster Alvord Endowed Fund in Neuropathology; Cure Alzheimer’s Fund.







