Declining nutrient intake in Reproductive-Age women

Groundbreaking study reveals how chromatin and DNA methylation changes during brain development contribute to the risk of neuropsychiatric disorders like schizophrenia and bipolar disorder.
Study: Macronutrient and Micronutrient Intake Among US Women Aged 20 to 44 Years. Image Credit: Marina Litvinova / Shutterstock.com
A recent study published in JAMA Network Open compares trends in nutrient consumption from dietary sources and supplements in pregnant and non-pregnant women in the United States.
The impact of nutrient deficiencies during pregnancy
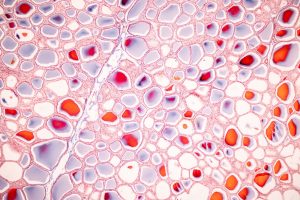
Nutritional status is crucial for maternal health and fetal growth, as it reduces the risk of chronic diseases in later life.
Energy requirements are greater during pregnancy due to increased metabolic processes and workload on the lungs and the heart. During pregnancy, women require multiple nutrients, including protein for tissue growth, iron to produce red blood cells, folate to prevent neural disorders, calcium to develop strong fetal bones, and iodine for increased thyroxine secretion.
Several studies have reported inadequate nutrient intake among pregnant women in the United States, with a high prevalence of magnesium, vitamin D, and vitamin E deficiencies. Pregnant women also consume less potassium, choline, and vitamin K, despite higher rates of nutrient supplementation than non-pregnant women. Furthermore, most pregnant women consume eicosapentaenoic acid (EHA) and docosahexaenoic acid (DHA) below the recommended threshold for optimal health.
About the study
The current study, which was conducted between February 2022 and July 2024, included 1,392 pregnant and 9,737 non-pregnant women between 20 and 44 years of age. Data were obtained from at-home interviews and visits to mobile examination centers.
Study participants provided one or more 24-hour dietary recalls at mobile examination centers, followed by telephonic conversations. The study participants also provided information on their age, race, ethnicity, education, smoking status, and income-to-poverty ratio (PIR).
Pregnancy status was determined from positive urine pregnancy tests and self-reported trimester. The primary study measures included the average regular consumption of micronutrients and macronutrients, as well as the prevalence of micronutrient intake insufficiency. The U.S. Food Security Survey Module was utilized to assess adult food security.
Participant enrollment in the Food Stamps, Supplemental Nutrition Assistance Program (SNAP), and Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) was also recorded. Program enrollment was based on benefits received in the previous year.
Data were also analyzed from ten National Health and Nutrition Examination Surveys (NHANES) cycles between 1999 and 2018. The National Cancer Institute (NCI) approach and linear regressions enabled the analysis, whereas the Simulating Intake of Micronutrients for Policy Learning and Engagement (SIMPLE) tool evaluated nutrient intake.
Trends in supplement use and dietary intake
The mean age of pregnant and non-pregnant women was 29 and 32 years, respectively. Among pregnant women, 27% and 34% were in their first and second trimesters, respectively.
Dietary supplement use was significantly higher among pregnant women than non-pregnant women at 78% and 46%, respectively. The mean carbohydrate consumption reduced from 307 g/day during 1999-2000 to 275 g/day during 2013-2018 among pregnant women. Among non-pregnant women, carbohydrate intake reduced from 252 g/day to 217 g/day from 1999-2000 to 2017-2018.
Between 1999-2000 and 2013-2018, an 11 percent point (pp) increase was observed in pregnant women who consumed below the Estimated Average Requirement (EAR) of vitamin A. The percentage of pregnant women who consumed below-EAR vitamin C also increased by 8.9 pp. Likewise, the percentages of non-pregnant women with insufficient consumption of vitamin A, vitamin C, and iron increased by 20, 11, and five pp, respectively, from 1999-2000 to 2017-2018.
The average calcium consumption increased from 1,121 mg/day to 1,309 mg/day for pregnant women and from 850 mg/day to 981 mg/day for non-pregnant women. Among pregnant women, prevalence rates for insufficient intake were reduced by 16 pp for magnesium and 33 pp for vitamin K. Among non-pregnant women, insufficient consumption reduced by 16 pp of calcium, 16 pp of magnesium, and 33 pp of vitamin K.
Pregnant women primarily reduced their carbohydrate intake from added sugars, fortified flour, and cereals. Health professionals advise limiting sugar intake; however, reducing fortified flour and cereal consumption could reduce the intake of vitamins A, C, magnesium, iron, and folate.
Decreased use of supplements due to side effects like nausea and constipation could further reduce iron intake. Furthermore, reduced vitamin C intake may exacerbate iron inadequacy.
Conclusions
Carbohydrate, vitamin A, vitamin C, and iron intake has reduced in the past two decades among pregnant and non-pregnant women in the U.S. The nutrient gaps identified in the present study could inform regulatory, healthcare, and scientific communities to formulate policies and guidelines to improve nutrient intake by reproductive-age women in the U.S..
Journal reference:
- Miketinas, D., Luo, H., Firth, J. A., et al. (2024). Macronutrient and Micronutrient Intake Among US Women Aged 20 to 44 Years. JAMA Network Open 7(10). doi:10.1001/jamanetworkopen.2024.38460