Fine Particulate Matter and Gestational Diabetes Risk

A recent BMC Public Health study assesses the relationship between exposure to fine particulate matter (PM2.5) and the risk of gestational diabetes mellitus (GDM).
Study: The impact of PM2.5 and its constituents on gestational diabetes mellitus: a retrospective cohort study. Image Credit: chayanuphol / Shutterstock.com
Does PM2.5 pollution cause GDM?
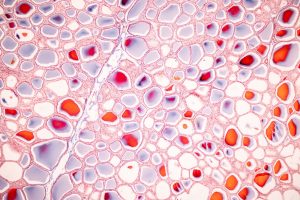
The incidence of GDM, which is a common metabolic disorder of pregnancy, has increased in recent years. It is imperative to study the pathogenic factors contributing to the risk of GDM, as this condition affects the health of pregnant women and increases the risk of adverse pregnancy outcomes, such as neonatal hypoglycaemia and macrosomia.
The mechanisms through which PM2.5 and its constituents lead to GDM remain unclear. Current evidence suggests that the polycyclic aromatic hydrocarbons (PAHs) present in PM2.5 may contribute to insulin resistance (IR) by suppressing the insulin receptor substrate 2 gene. PM2.5 also alters the CC-chemokine receptor 2 signaling pathway, which exacerbates IR.
However, some studies have also indicated the lack of an association between GDM and PM2.5 also exists. Thus, large-scale studies are needed to elucidate the potential association between PM2.5 exposure and the risk of GDM.
PM2.5 comprises various substances, such as sulfate, nitrate, organic matter (OM), ammonium, and black carbon (BC), with varying toxicity associated with each of these components. For example, one study reported ammonia to be the main cause of asthma, whereas another study identified OM as the primary chemical responsible for the increased risk of diabetes mellitus due to PM2.5 exposure.
To date, few studies have examined the association between GDM risk and PM2.5 and its constituents.
About the study
The current retrospective study included pregnant women from Guangzhou City, Guangdong Province, China to document the associations between PM2.5 and its constituents and the risk of GDM. Data were obtained between 2020 and 2022 from a local hospital and the 10th revision of the International Classification of Diseases (ICD-10) definition was used to diagnose GDM.
All study participants conceived naturally, lived in Guangzhou during pregnancy, had complete data, were not pregnant with twins, and did not have a history of hypertension or diabetes before pregnancy.
The Tracking Air Pollution in China (TAP) project database was used to obtain information on the daily concentrations of PM2.5 and its constituents. Data were also compiled on potential confounding factors such as age, ethnicity, marital status, occupation type, and blood type.
To diagnose GDM, women completed an oral glucose tolerance test, which was administered after fasting for at least eight hours between the 24th and 28th weeks of pregnancy.
Study findings
A total of 17,855 pregnant women were included in the study, 22.1% of whom were diagnosed with GDM. The median age of the participants was 29 years, about 15% of whom were of an advanced maternal age.
Median exposure concentrations for PM2.5, sulfate, and OM in the GDM group were higher as compared to the non-GDM group. A strong correlation was observed among the concentrations of PM2.5, OM, BC, sulfate, nitrate, and ammonium. The robustness of the correlations was established by removing outliers and conducting a sensitivity analysis.
After adjusting for confounding factors, exposure to higher concentrations of PM2.5 in the first trimester was associated with an increased risk of GDM by 9.2%. When stratified by PM2.5 constituents, the increased risk of GDM for sulfate, nitrate, ammonium, OM, and BC was 8.6%, 11.6%, 11.1%, 9.7%, and 8.5%, respectively.
Exposure to PM2.5, sulfate, nitrate, ammonium, OM, and BC between the first and second trimesters, as well as exposure to PM2.5, nitrate, ammonium, and OM in the second trimester, also increased the risk of GDM.
After adjusting for confounding factors, the inflection points between PM2.5, OM, and BC concentrations and GDM risk were lowest in the second trimester. Furthermore, the inflection points between sulfate, nitrate, and ammonium concentrations and GDM risk were lowest in the first to second trimester. The relationship between OM, ammonium, nitrate, and PM2.5 exposure and GDM risk in the first trimester was non-linear.
Significant associations were observed between PM2.5, nitrate, sulfate, ammonium, OM, and BC exposure and GDM risk in the anemic, non-primiparous, and infant sex subgroups. A pattern of higher GDM risk was also observed between the first and second trimesters, as well as the second trimester subgroup. An interaction by age subgroup was observed only between exposure to OM, sulfate, and BC in the first trimester and GDM risk.
Conclusions
Exposure to BC and sulfate in during the second trimester is negatively associated with GDM risk, whereas exposure to PM2.5 and its constituents during other stages of pregnancy was associated with an increased risk of GDM. The identification of these crucial inflection points has important implications for public health interventions that can be developed to prevent GDM.
Journal reference:
- Liu, W., Zou, H., Liu, W., & Qin, J. (2024) The impact of PM2.5 and its constituents on gestational diabetes mellitus: a retrospective cohort study. BMC Public Health. 24, 2249. doi:10.1186/s12889-024-19767-1