Immune boost may protect against multiple hospital-acquired infections
At a Glance
- A novel type of vaccine designed to stimulate the innate immune system provided protection for mice against a wide range of bacteria and fungi.
- If effective in people, the approach could help prevent deaths from hospital-acquired infections caused by a variety of treatment-resistant microbes.
Every year, more than 700,000 people in the U.S. catch infections in hospitals and other healthcare facilities. These infections are often caused by microbes that are resistant to treatment. More than 90,000 people die of such infections each year, despite modern sanitary techniques to stop their spread.
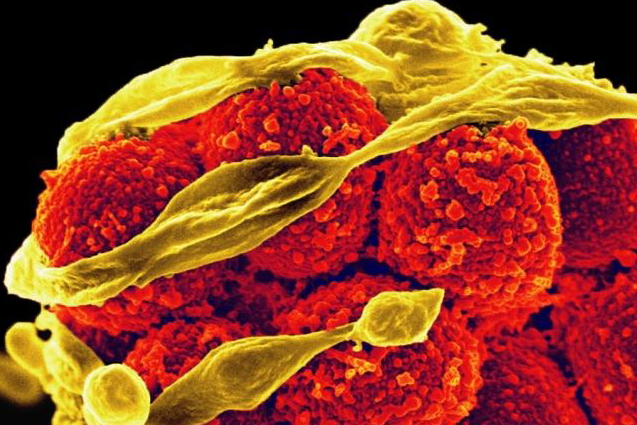
Prevention is also tough because many different bacteria and fungi can cause hospital-acquired infections. New antimicrobial drugs are difficult to develop, and designing individual vaccines to prevent the spread of each type is impractical. Traditional vaccines teach the body’s adaptive immune system—which includes antibodies, T cells, and B cells—to recognize and remember a protein from a single type of microbe.
An alternate approach would be to try to stimulate the innate immune system. This is the body’s early warning system. Its cells constantly move through the body searching for signs of damage or infection. Unlike the adaptive immune system, this first line of the body’s defense doesn’t keep long-term memories of specific pathogens. However, recent studies revealed that innate immune cells do keep a kind of memory, lasting weeks to months, that allows them to react more effectively the second time they encounter a pathogen.
This discovery raised the possibility that a vaccine might be designed to broadly activate innate immune cells to defend the body during times of high infection risk. In a new study, researchers designed protein-free vaccines to boost the innate immune system and tested them in mice. The team was led by Jun Yan and Dr. Brad Spellberg at the University of Southern California and funded in part by NIH. Results were published on October 4, 2023, in Science Translational Medicine.
The original vaccine the team tested included three substances known to boost general immune responses: aluminum hydroxide, monophosphoryl lipid A (MLP), and whole glucan particles. When given to mice several days before exposure, the vaccine protected against death from a bloodstream infection of methicillin-resistant Staphylococcus aureus, or MRSA. But it didn’t protect against death from pneumonia caused by another bacteria.
The team then tested the addition of a complex sugar molecule called mannan, which is found in many fungi and known to be a potent stimulant of the immune system. When whole glucan particles were replaced with mannan, the vaccine protected mice against death from several different microbes delivered to either the bloodstream or the lungs.
When mice were immunized with high doses of the vaccine, it provided protection within 24 hours and for up to 28 days. After a booster shot, protection returned for several additional weeks. In follow-up experiments, the researchers found that monocytes and macrophages—crucial players in the innate immune defense against pathogens—were required for this protection.
Further work showed that the vaccine induced certain changes in gene activity in these immune cells. Overall, this created a less inflammatory response to infection. Less inflammation can reduce the risk of sepsis—a deadly response of the body to some hospital-acquired infections. Finally, in preparation for human testing, the team showed that human macrophages had the same gene activity changes when exposed to the vaccine.
“This is very different from developing new antibiotics,” Yan says. “This is using our own immune system to fight against different superbugs.”
Aluminum hydroxide and MLP are already used in FDA-approved vaccines. The researchers are currently planning how to test the vaccine in human volunteers.
—by Sharon Reynolds
References: A protein-free vaccine stimulates innate immunity and protects against nosocomial pathogens. Yan J, Nielsen TB, Lu P, Talyansky Y, Slarve M, Reza H, Novakovic B, Netea MG, Keller AE, Warren T, DiGiandomenico A, Sellman BR, Luna BM, Spellberg B. Sci Transl Med. 2023 Oct 4;15(716):eadf9556. doi: 10.1126/scitranslmed.adf9556. Epub 2023 Oct 4. PMID: 37792959.
Funding: NIH’s National Institute of Allergy and Infectious Diseases (NIAID); National Health and Medical Research Council.








