NIH clinical trial will test precision medicine treatments for myeloid cancers
News Release
Wednesday, October 23, 2024
Researchers will seek to accelerate the discovery of more tailored treatments for these aggressive cancers of the blood and bone marrow.
The National Institutes of Health (NIH) has launched a proof-of-concept precision medicine clinical trial to test new treatment combinations targeting specific genetic changes in the cancer cells of people with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS). The trial, funded by NIH’s National Cancer Institute (NCI), aims to accelerate the discovery of more tailored treatments for these aggressive cancers of the blood and bone marrow.
“NCI is uniquely positioned to conduct this type of study, which is one of a series of NCI precision medicine trials that are helping pave the way for more personalized treatment of cancer,” said W. Kimryn Rathmell, M.D., Ph.D., director of NCI. “By making these trials available to patients in communities around the country, we bring cutting edge science to people where they live and ensure that what we learn from our study participants can benefit patients like them in the future.”
“AML and MDS are a heterogeneous group of cancers that can progress very quickly. Treatment advances depend in part on the ability to rapidly identify which subtype of cancer each patient has so that treatments can be tested for their specific cancer,” said Richard F. Little, M.D., of NCI’s Division of Cancer Treatment and Diagnosis. Dr. Little is the NCI coordinator for the trial, known as the Myeloid Malignancies Molecular Analysis for Therapy Choice (myeloMATCH). “The goal of myeloMATCH is to test combinations of drugs to treat the disease in a highly targeted way and to be able to start treatment quickly after diagnosis.”
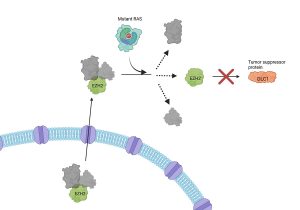
Initially, people enrolled in the trial with newly diagnosed AML or MDS will undergo rapid genetic testing of their tumor samples. Based on the molecular characteristics of their tumors, they will be matched to a substudy testing a treatment appropriate for the specific genetic changes and characteristics associated with their disease, if one is available, or to standard treatment if an appropriate substudy is not available.
If the initial treatment works to reduce a patient’s disease, they will undergo further genetic testing to match them to a subsequent substudy testing a treatment that is appropriate for the specific genetic changes associated with their remaining disease. As the amount of a patient’s disease decreases, study investigators will use increasingly sensitive tools, such as biomarker assays, to identify appropriate treatments for any remaining cancer cells.
The myeloMATCH trial aims to enroll several thousand people within the first few years, with new substudies rolled out over time. Blood and bone marrow samples collected from participants during the course of the trial will be used to develop and refine the assays, as well as understand what genetic changes might be associated with the development of resistance to a treatment.
myeloMATCH is being conducted by the National Clinical Trials Network, with the participation of the NCI Community Oncology Research Program (NCORP). Initial substudies will be led by the SWOG Cancer Research Network, the Alliance for Clinical Trials in Oncology, the ECOG-ACRIN Cancer Research Group, and the Canadian Cancer Trials Group. The Frederick National Laboratory for Cancer Research, Fred Hutch Cancer Center, and Children’s Hospital Los Angeles will provide clinical laboratory support for the substudies.
myeloMATCH is one of three next-generation precision medicine trials that NCI has under way. ComboMATCH is testing the effectiveness of treating adults and children who have relapsed solid tumors with new drug combinations that target specific tumor alterations. ImmunoMATCH has launched a pilot study to determine whether prospective characterization of the immune status of a tumor can be used to improve the response to targeted immunotherapy treatments, with plans to expand to larger studies in the future.
All three trials are successors to NCI-MATCH, NCI’s groundbreaking precision medicine clinical trial, which showed that people with advanced cancer may benefit from genomic sequencing to help plan their treatment.
“When President Biden and the First Lady re-ignited the Cancer Moonshot, they set two clear goals: To prevent more than 4 million cancer deaths by 2047 and to improve the experience of people who are touched by cancer,” said Danielle Carnival, deputy assistant to the President for the Cancer Moonshot. “To achieve that goal, the U.S. government is working to expand access to innovative trials like this one, bring targeted new treatments to patients, and, ultimately, save lives.”
Learn more about myeloMATCH and the substudies that are currently open.
About the National Cancer Institute (NCI): NCI leads the National Cancer Program and NIH’s efforts to dramatically reduce the prevalence of cancer and improve the lives of cancer patients and their families, through research into prevention and cancer biology, the development of new interventions, and the training and mentoring of new researchers. For more information about cancer, please visit the NCI website at www.cancer.gov or call NCI’s contact center, the Cancer Information Service, at 1-800-4-CANCER (1-800-422-6237).
About the National Institutes of Health (NIH):
NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
NIH…Turning Discovery Into Health®