Study shows radial arterial access superiority in coronary interventions
New data demonstrate the superiority of radial arterial access compared to femoral arterial access for coronary interventions. Findings showed radial access was associated with lower rates of in-hospital mortality, major access bleeding, and other major vascular complications compared with femoral access. The late-breaking results were presented today at the Society for Cardiovascular Angiography & Interventions (SCAI) 2024 Scientific Sessions.
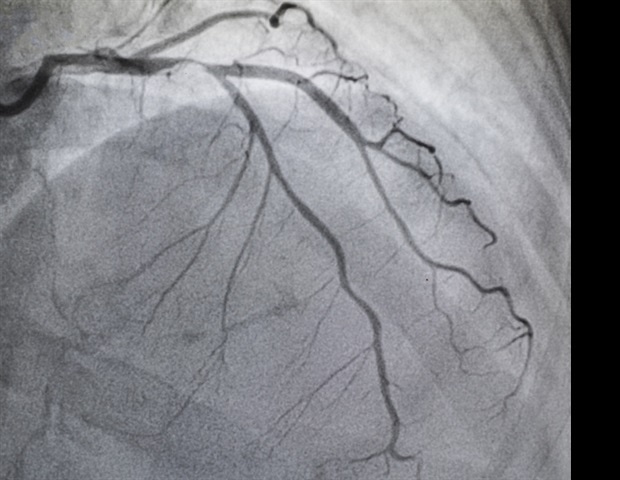
Historically, femoral arterial access, through the groin, for percutaneous coronary intervention (PCI) was the standard. Radial access, or the use of the radial artery in the wrist as the entry point for the catheter, is an alternative and provides potential benefits, such as reduced bleeding complications, infection rates, and readmissions. While recent research supports these advantages, the broader adoption of transradial PCI in the U.S. is unknown.
The retrospective cohort study used data from the National Cardiovascular Data Registry’s CathPCI Registry including PCIs performed between 2013 and 2022. The comparative safety of radial versus femoral access for PCI was evaluated using instrumental variable analysis exploiting operator variation in access preferences.
During the study period, 6,658,479 PCI procedures were performed, of which 40.4% (n= 2,690,355) were performed via radial access, increasing from 20.3% in 2013 to 57.5% in 2022, representing a 2.8-fold increase over the past decade. This increase was seen in all geographic regions and across the full spectrum of presentations, with the largest relative increase seen in patients with ST-segment elevation myocardial infarction.
2,244,115 PCIs met inclusion criteria for the instrumental variable analysis, which showed radial access was associated with lower in-hospital mortality (absolute risk difference [ARD] of -0.15%, P< 0.001), major access site bleeding (ARD of -0.64%, P< 0.001), and other major vascular complications (ARD of -0.21%, P< 0.001) but a higher risk of ischemic stroke (ARD of 0.05%, P< 0.001). There was no association with the falsification endpoint of gastrointestinal or genitourinary bleeding (P= 0.89).
The study demonstrates a sea change in the manner in which PCI is performed in the US in response to trial data but also highlights the continued opportunity for practice improvement with dramatic interoperator variation. It confirms that the benefit observed for radial access in RCTs has also been seen in real-world practice, including the largest benefits for the highest-risk patients. Finally, it shows a highly credible novel finding in the increased in stroke risk.”
Reza Fazel, MD, FSCAI, cardiologist at Beth Israel Deaconess Medical Center and lead author of the study
Session details:
- “Temporal Trends and Clinical Outcomes with Radial Versus Femoral Arterial Access for Percutaneous Coronary Intervention in the United States”
- Friday, May 2, 2024; 9:17-9:24 AM PT
- Long Beach Convention Center, 104A, First Level








