The Impact of Overuse of Preventative Blood Thinners: A Pilot Study
A year-old pilot project at St. Paul’s Hospital to track unnecessary use of preventative blood thinners in hospital patients has seen a decline in use by 53 per cent.
The Anticoagulation Stewardship Program (ACSP) is the first in British Columbia and Canada to focus on these preventative blood thinners, known as heparin medications, with a view to reducing inappropriate use.
By extension, the ACSP also aimed to decrease associated drug costs, negative health effects on patients, and nursing workloads.
Pilot exceeds goals
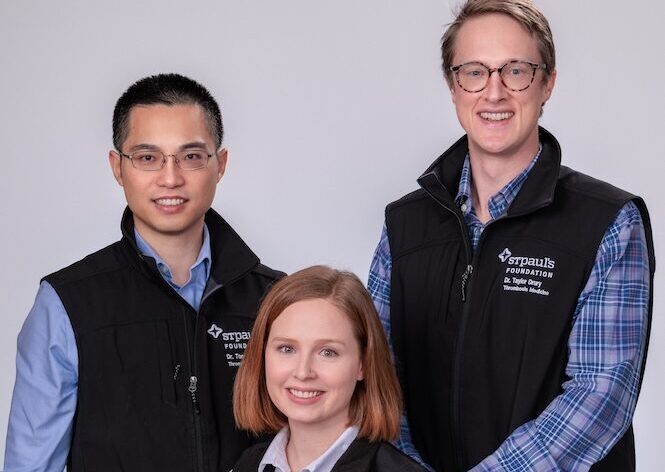
The pilot, a collaboration with thrombosis specialists and Providence Health pharmacy support services, has met and even exceeded its goals, says Dr. Tony Wan, who leads the ACSP with fellow thrombosis physician Dr. Taylor Drury and Dr. Stephanie Garland, Clinical Pharmacy Specialist in hematology and thrombosis at Providence.
Hospitalized patients have a higher risk of blood clots because they are less active than usual. So, the current practice is to prescribe most patients with injectable heparin medications to prevent against clots.
Overuse affects patients, health care workers, budgets
“Most people who get admitted to hospital receive heparin,” says Dr. Wan. “Surgery patients in particular do, but so do people coming in for a range of medical illness, from minor infections to diabetes to kidney
diseases.”
Dr. Wan knew that data and research show that overprescribing has had negative effects on patients, health-care workers, and health-care budgets. The cost of heparin meds in 2022 at St. Paul’s Hospital alone was almost $280,000.
Preventative heparin medications needed a big rethink, he says, especially since the risk of a clot forming in most hospitalized medical patients is relatively small, occurring in just one per cent of low-risk patients. Meanwhile, a major risk of blood thinners is excess bleeding, in addition to the pain and discomfort from receiving the daily injection.
Tool calculates clot risk
Key to the program was identifying patients who were at low risk of developing clots. Pharmacist Dr. Garland was funded to work on the pilot for half of her time and used a tool, tested on a large group of patients, to determine risk. It factored in a person’s previous history of clots, cancer or paralysis of lower limbs, along with mobility levels and age. (Clotting risks increase in those over 60.)
Patients whose risk was calculated at one per cent or less were considered low. A higher-percentage risk was considered moderate to high.
The pilot started with patients in St. Paul’s Medicine, Urban Health and Acute Care for Elderly units, which, combined, have 165 beds.
Dr. Garland reviewed patient charts to calculate their risks, then advised their doctor accordingly. The doctor had discretion in heeding the
recommendation or not.
“We are a consulting service, so we don’t change orders unless the most responsible physician is involved,” says Dr. Garland. “We leave notes in the chart. Physicians have the choice to agree or not.”
In the first few months since the pilot launched in January 2023, about 60 per cent of the time, doctors accepted the pharmacist’s recommendations. After six months, that number increased to about 80 per cent, reports Dr. Wan.
Chart screening to determine clot risk resulted in 11,000 fewer heparin injections used in the year.
Reduced heparin prescribing resulted in a yearly savings of $75,000 to the hospital, which exceeded the cost of half of a pharmacist’s salary.
Serious heparin side effects decreased
A significant patient benefit was a reduction in a serious condition called heparin-induced thrombocytopenia (HIT). It is caused by an exposure to heparin and ironically, it causes clots instead of thinning the blood. The estimated risk of HIT is about 0.2 per cent from the use of enoxaparin, the most-used heparin medication in the hospital. HIT carries a 10-to-20 per cent mortality rate while many who survive are left with serious, permanent disabilities such as leg amputation.
More nursing time for patients
More selective administering of heparin resulted in big time savings for nurses. They spend about 5.5 minutes per injection, according to the pilot’s data. That equates to about 20 extra minutes a day in their schedule that could be spent providing other types of patient care. The pilot resulted in 1388 nursing hours saved in the year.
With each nursing shift lasting 12 hours, that extra time could free up 115 more shifts, helping to ease nursing demand.
That wasn’t the only nursing benefit. Another was their improved safety. Dr. Wan explains that 90 per cent of nurses surveyed experienced verbal or physical violence when administering the sometimes-painful injection, which is usually given in the evening when patients might be tired and sleepy. “Many elderly patients may be confused or delirious at that time of day,” Dr. Wan adds.
Artificial intelligence could play role
With all these benefits, the pilot’s leaders would like to grow it to all in-patient units at St. Paul’s and at Mount Saint Joseph Hospital. That would require more pharmacist support, but the program is currently investigating the role that artificial intelligence (AI) could play in performing some of the screening tasks the pharmacist performs. This would allow for a larger number of patients to be screened with the same amount of pharmacist time.
Donors to St. Paul’s Foundation and The Department of Medicine (DOM) Innovation Platform provided support to the pilot.
By Ann Gibbon
Ann Gibbon works in communications at Providence Health Care, Vancouver.








