Use These Antibiotics for Close Contacts of Invasive Meningococcal Disease, CDC Says
Rifampin, ceftriaxone, or azithromycin are recommended as first-line alternatives to ciprofloxacin prophylaxis for close contacts of people with meningococcal disease in areas where the disease is highly resistant to ciprofloxacin, according to new guidance from the CDC.
Health departments should consider using other antibiotics for prophylaxis when, over the course of the past 12 months, there have been 1) two or more invasive meningococcal disease cases caused by ciprofloxacin-resistant strains in the local catchment area, and 2) 20% or more of all reported invasive meningococcal disease cases in that area are caused by ciprofloxacin-resistant strains, Isha Berry, PhD, of the agency’s National Center for Immunization and Respiratory Diseases in Atlanta, and colleagues wrote in the Morbidity and Mortality Weekly Report.
In addition, the CDC advised health departments to maintain the updated prophylaxis approach until a full 24 months had passed without any reported invasive meningococcal disease cases due to ciprofloxacin-resistant strains in the catchment area, defined as a single contiguous area including all counties reporting the resistant cases.
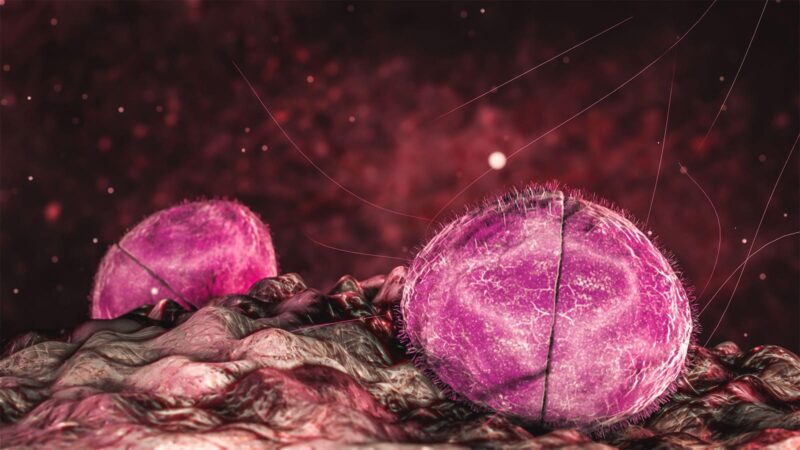
Neisseria meningitidis, the causative agent of invasive meningococcal disease in the U.S, has generally been susceptible to ciprofloxacin, however ciprofloxacin-resistant cases have been on the rise in recent years, and relying on ciprofloxacin for prophylaxis in these areas could result in prophylaxis failure, they warned.
In the U.S., there was an annual average of 1.25 cases of invasive meningococcal disease caused by ciprofloxacin-resistant strains from 2011 to 2018. But, during 2019, 2020, and 2021, that number rose to an annual average of 9.7 cases, Berry and colleagues wrote, despite a 75% decline in incidence of the disease from 2011 to 2021.
Of note, ciprofloxacin- and penicillin-resistant NmY strains caused most of the recent cases. Geographically, these cases occurred throughout the U.S., although there were clusters in certain areas, most notably New Mexico and California.
Because the CDC is responsible for monitoring and reporting on antimicrobial susceptibility testing for N. meningitidis, susceptibility testing isn’t usually conducted by local health departments or as part of patient care. This means that results of susceptibility testing don’t usually guide individual choice of antimicrobial prophylaxis for close contacts of affected patients. However, if information on susceptibility is available through local testing, prophylaxis can be adjusted, regardless of the proposed CDC thresholds, the authors noted.
To arrive at its recommendations for alternative antibiotic choices, the CDC relied on the results of a 2013 systematic review and meta-analysis that looked at the efficacies and safety profiles of antibiotics for the prevention of meningococcal infections. The meta-analysis found that rifampin was effective at eradicating N. meningitidis a week after prophylaxis (RR 0.17, 95% CI 0.13-0.24). Two studies included in the review compared rifampin with ceftriaxone and found no statistically significant difference in eradication (RR 3.71, 95% CI 0.73-18.86). Another study that compared azithromycin to rifampin also reported no statistically significant difference in eradication (RR 0.30, 95% CI 0.30-5.54).
Ongoing monitoring for antibiotic resistance of meningococcal isolates through surveillance and healthcare providers’ reporting of prophylaxis failures will guide future updates to prophylaxis considerations and recommendations, the authors concluded.
Disclosures
Berry and other authors reported no potential conflicts of interest.
Primary Source
Morbidity and Mortality Weekly Report
Source Reference: Berry I, et al “Selection of antibiotics as prophylaxis for close contacts of patients with meningococcal disease in areas with ciprofloxacin resistance — United States, 2024” MMWR 2024; DOI: 10.15585/mmwr.mm7305a2.








