What to consider before embarking on a specialist career
Amardip Kalsi explains how he embarked on his specialist career and offers invaluable advice to younger dentists who may be considering how best to approach their own career pathways in dentistry.
Tell us about your career; why you chose dentistry and what led you to your current position?
When I initially considered what kind of career to pursue, I knew I wanted to do something vocational, with a pathway ahead of me.
What I liked about dentistry was the idea of being a leader of a small team, and the idea of working in a hands-on, operative and clinical environment of patient interaction and helping people, rather than in an office-based job.
Why did you decide to specialise and what has this meant for your career pathway?
I had a few training posts in hospital, plus some experience in practice, and found I was still keen to learn and develop more.
I considered doing short, postgraduate training, such as a Master’s but decided I’d rather undertake specialist training because one, I’d be on the specialist list and two, it would give me a more robust and rounded approach rather than training that covered specific aspects of certain parts of dentistry.
Restorative dentistry also really stood out to me as a specialty; I thought that the role of a consultant would suit me and I liked the prospect of working in a multi-disciplinary team environment, which is challenging but incredibly interesting and rewarding at the same time.
Why did you choose the dental hospital route rather than practice?
I just found it a very stimulating environment to work in, and by the end of foundation training, I felt that if I were going to stay in practice I would be working in one room every day with the same person.
By contrast the hospital environment lends itself to drawing on input from a lot of different people and to seeing – and tackling – rarer and complex cases.
Why has restorative dentistry been your main focus?
I like how broad it is as a specialty, but also specifically the interface between prosthodontics and periodontics and how that can apply to complex cases.
I like the high level of detail with a broad overview, which is very stimulating, holistic, whole mouth dentistry, where you look at all the different facets of a case and then assess from there exactly what needs to be done – and then deliver it. It is seeing something through from start to finish.
In what way can your leading roles in restorative dentistry help the younger generations and what has encouraged you to take teaching and mentoring roles?
Teaching helps me to stay fresh myself, because these days there’s so much clinical evidence and so many new techniques being developed all of the time, so it enables you to sit down and analyse things in a great deal of detail.
Mentoring specifically is an enjoyable way to see people develop: while teaching is imparting information, mentoring is very much about helping, supporting, and guiding people to access information and to develop themselves.
It’s also important to advocate for people who are training and developing, and help them navigate their career pathways.
My role has also led to interactions with national organisations; and I also created a guidance document for postgraduate training in restorative dentistry for the British Society for Restorative Dentistry with input from some of my mentors.
Amardip’s top five tips for young dentists
- In any situation, whether clinical, non-clinical, or something completely outside of dentistry, take time to identify the challenges and then develop strategies to tackle them
- Always think through the options, so it takes the guesswork out of making a decision
- Keep your options open wherever you can, especially in relation to postgraduate training in restorative dentistry. Do as many different courses as you can so that pathways are open to you should you wish to pursue them further
- If an opportunity presents itself, take it if you can (as long as it’s sensible!)
- Finally, always remember the patient. Do what’s best for them and that will keep you in good stead.
Tell us more about the guidance document you produced for postgraduate training in restorative dentistry. How is it different from other guidance, and what was your ambition for it?
The difference between this and other guidance is that it appreciates that restorative dentistry is a broad umbrella term rather than just focusing on the restorative dentistry registrar specialty training pathway. I also created it because the specialty of restorative dentistry is unique to the UK and is not well understood.
It also covers a lot of the questions that people have about the different career pathways, from short courses to boost skills and clinical techniques, to going down the full route of specialty training or following an academic pathway to a PhD.
What defines a successful course to ensure delegates really take away key tips they can implement quickly and safely in a practice setting?
A successful course is one where people can quickly just start applying whatever they’ve learned and do that effectively and safely. The key for that is something called deep learning; a learning and teaching concept, which relates to how information is consolidated within your mind.
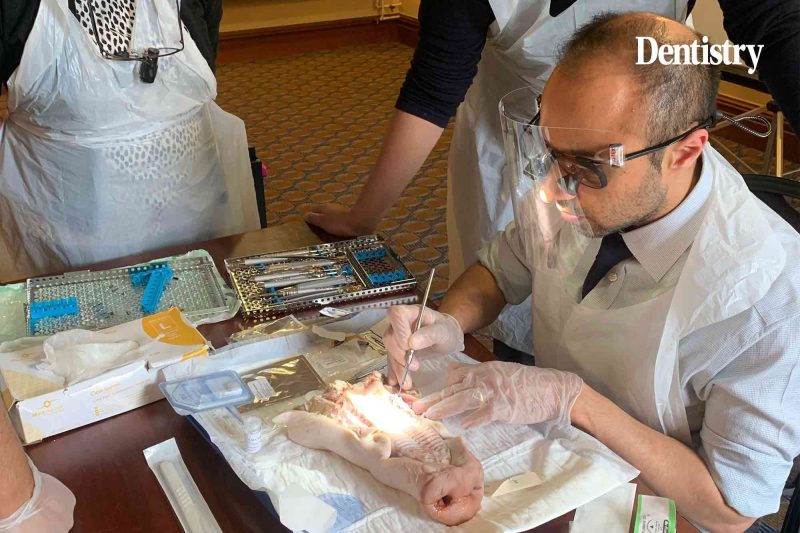
Why do you train using human cadaver heads and pigs’ heads over phantom heads?
As a clinician, you are as good as the amount of experience that you have. So, the more often you perform a specific procedure, the better you’re going to be at it.
Cadaver heads are the closest simulation that you will ever get to operating surgically, and while pigs’ heads are not to the same level of detail, for a lot of procedures, they are the next best thing to help develop specific skills. The rationale is to build as many hours of experience as possible in as close a simulation to the real world as possible.
What advice would you give to young dentists?
My advice would be to be self-critical and to take on criticism as best as you can while taking the emotional aspect of this out of it, because that’s the only way to improve and we all need to improve. Look for ways to continually learn as much as you can.
How do you see restorative dentistry in the future?
The big thing will be artificial intelligence. We’ve already had CAD/CAM processes that are increasingly widely used, and coupled with AI will hopefully take some of the burden of clinical and technical work.
We also have an aging population presenting with complex needs, while on the other hand, the younger generation needs less of the traditional types of dentistry.
We will see more of a focus on procedures which are to idealise the oral situation, rather than dealing with caries and periodontal disease in younger cohorts whilst the older cohorts will require more complex care.







